Normal Values
If a normal value for CFVR should be defined, then the cut-off value of 2 must be accepted, because it has been demonstrated in various studies that CVFR <2 detects epicardial coronary artery stenosis and predicts myocardial ischaemia in the underlying territory.7,19,20 The sensitivity and specificity for the cut-off value of <2 CFVR to detect significant LAD stenosis are both more than 90 %.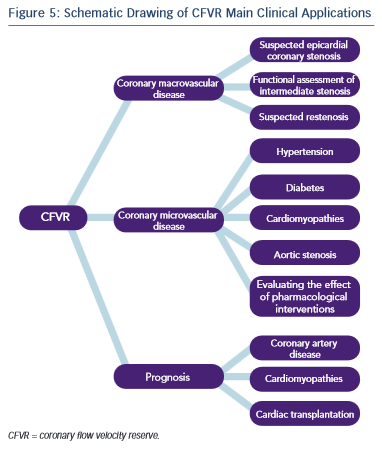
In the setting of normal epicardial coronary arteries CFVR assesses coronary microcirculatory function and in this setting ‘normal’ CFVR values vary significantly according to the studied population,21–23 presence and extent of atherosclerostic risk factors,24,25 concomitant therapy,21,26 etc. Ageing also affects CFVR – baseline flow velocity increases with age, while maximal hyperaemic flow does not change and therefore CFVR value decreases with advancing age.27
Therefore in a clinical setting and in a study population a more useful way to interpret CFVR values is to compare CVFR before and after an event or therapeutic intervention, or to a control group, instead of using pre-defined cut-off values.
Clinical Application
Given the physiological basis of CFVR measurement the method has two major areas of application: evaluation of epicardial coronary artery stenosis and assessing microvascular myocardial function in the absence of epicardial stenosis (see Figure 5).
CFVR could be useful as a diagnostic and prognostic tool in different clinical situations, such as the diagnosis of functionally significant coronary stenosis, evaluation of patients with intermediate coronary stenosis, follow-up after percutaneous coronary intervention (PCI), coupling left ventricular function with perfusion during stress echocardiography, evaluation of coronary microcirculation in the setting of hypertension, diabetes and other conditions, assessment of the effectiveness of certain therapeutic intervention and risk stratification in patients with dilated cardiomyopathy, after heart transplantation and other diseases.
Focusing the attention on patients with suspected or proved coronary artery disease, a practical guide to the application of CFVR is as follows:3
1.Before coronary angiography
a.Suspected epicardial coronary stenosis (CFVR combined with wall motion score).
b.Suspected microvascular abnormalities (CFVR in LAD).
2.After coronary angiography
a.Abnormal coronary angiogram – functional assessment of intermediate stenosis (CFVR combined with wall motion score).
b.Normal coronary angiogram – confirmation or exclusion of microvascular dysfunction (CFVR in LAD).
3.Follow-up after initial coronary angiogram
a.Follow-up of functional significance of intermediate stenosis (CFVR combined with wall motion score).
b.Patients with suspected restenosis (CFVR combined with wall motion score).
c.Verification of beneficial effect of pharmacological interventions (CFVR in LAD).
Coronary Artery Stenosis
Evaluation of patients with coronary stenosis in the range of 50–70 % is challenging. CFVR is a useful tool to assess the functional significance of the stenosis. When CFVR is <2 revascularisation could be safely deferred given the high negative predictive value of CFVR to detect ischaemia.20,28 The diagnostic accuracy of CFVR (adenosine) in three major coronary arteries for detecting ischaemia has been compared with FFR in a prospective study in 172 vessels of 140 patients with at least one ≥50 % stenosis in a major epicardial artery. A CFVR cut-off of 2.2 demonstrated high sensitivity and specificity to predict FFR ≤0.75.29
Percutaneous Coronary Interventions
Immediately after a PCI CFVR could be measured invasively with intracoronary Doppler. Surprisingly, however, these early (immediate) measurements have shown a high rate of impaired CFVR even in the absence of any residual angiographic stenosis.3 This could be explained by microvascular stunning due to microembolisation, thrombogenicity (thrombin release) and vasoconstriction (endothelin release), or to temporary reactive hyperaemia, which masks normal reserve. Therefore, invasive immediate-after-PCI CFVR measurement is not a reliable baseline reference value, which could serve for follow- up of patients and monitoring for restenosis. It is better to measure CFVR at least several days after PCI and here comes the role of the non-invasive, repeatable, inexpensive and accessible transthoracic Doppler echocardiography.
CFVR value <2 in LAD after PCI predicts the presence of restenosis with high sensitivity (from 78 to 89 %) and specificity (from 90 to 93 %).30–32
Using a cut-off CFVR value of 2 is useful in the setting of intermediate coronary stenosis or after PCI but a more sensitive way to follow-up the progression of an intermediate lesion or to detect restenosis is to evaluate the evolution of CFVR over time and to compare current values with a reference value established for the individual patient.2
The introduction of drug-eluting stents (DES) in the field of interventional cardiology has significantly reduced the rate of restenosis after PCI. DES, however, are associated with delayed healing, which could lead to vasodilator dysfunction and late stent thrombosis. It is of interest therefore to dispose of a reliable, repeatable, non-invasive and inexpensive method to monitor vasodilator function in this setting. In a recent small study in 24 patients with acute coronary syndrome and PCI with DES in LAD, 3 months after the index procedure CFVR measured with transthoracic Doppler echocardiography and with invasive thermodilution method showed good agreement, suggesting that the non-invasive CFVR measurement is a feasible and reliable method for assessment of vasodilator dysfunction after DES implantation33.