Physiopathological Heart – Brain Connection
There are three disorders through which vascular disease brings on mild cognitive decline or dementia: i) stroke, ii) small vessel disease, and iii) -amyloid depositions (A ) that contribute to neurodegenerative phenomena. (see Figure 1)
Stroke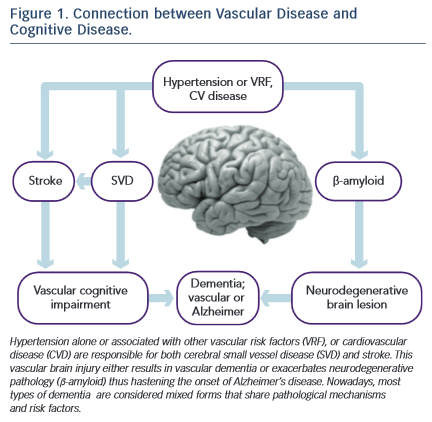
Fifty per cent of strokes may be attributed to hypertension, and they constitute the main risk factor for cognitive impairment or post-stroke dementia. The prevalence of post-stroke cognitive decline has a broad range, from 20 % to 80 %19. This variability depends on the diagnostic tools and the criteria employed, on the extent of the vascular and neurodegenerative pathologies before the stroke, on the cognitive status, on the stroke extension (volume) and topography (i.e. strategic areas such as frontal cortex, hippocampus or white matter).
Cerebral blood flow self-regulation alterations induced by brain ageing, vulnerability to hypoperfusion and hypoxia, lacunar infarcts (responsible for 70–90 % of vascular cognitive impairment), micro-haemorrhages, and neuron damage (protein synthesis and synaptic plasticity) account for the complex association between stroke and cognition.
Post-stroke cognitive status is not confined to vascular cognitive impairment or vascular dementia; it may also play a role in the genesis of Alzheimer’s disease and mood disorders (depression).
The Nun’s Study has shown that lacunar infarcts cause a 20-fold increase in the risk for Alzheimer’s disease20, and the PROGRESS Study (Perindopril Protection against Recurrent Stroke Study) has indicated that hypertension treatment reduces the risk for post- stroke dementia in 34 %21. Depression in older adults is closely related to subcortical vascular pathology, thus supporting the vascular depression hypothesis22. This syndrome presents a high post-stroke prevalence that ranges from 35 % to 50 %.
Small Vessel Disease
Small vessel disease is essentially associated with hypertension. The blood vessels supplying the white matter (penetrating arteries, branches of subarachnoid and subependymal arteries) are terminal arteries. The absence of collateral circulation renders the periventricular regions vulnerable to atherosclerotic ischaemic damage. The ischaemic episodes and the reactive gliosis lead to a process called araiosis (rarefaction) that damages the nerve myelin.
White matter hyperintensities (leucoaraiosis) and lacunar infarcts seen in neuroimages are the objective signs of these vascular abnormalities that cause white matter demyelination and subcortical-cortical disconnection or desaferentisation syndrome. The disconnection of the dorsolateral prefrontal cortex – the most affected circuit –gives rise to a cognitive syndrome called executive dysfunction, a distinctive feature of vascular brain injury and commonly seen in hypertensive patients23,24. On the other hand, selective neocortical atrophy (grey matter volume in the frontal lobes) may also contribute to the executive dysfunction25.
Our group has shown that patients with hypertension have a five-fold increased risk for executive dysfunction in the course of the disease26. Early detection of this syndrome is important because it increases the risk for conversion to dementia27 and/or to major depression22.
White matter disease, microinfarctions and micro-bleedings may have an impact on the onset of cognitive dysfunction. The volume or burden of white matter lesions, along with their progression and their location determine the clinical expression of the cognitive impairment and increase the risk for stroke. Limits to progression and burden depend on effective blood pressure control28.
β-amyloid depositions
β-amyloid is a protein that accumulates in brain extracellular spaces (neuritic plaques) and on the blood vessel walls (cerebral amyloid angiopathy). It results from the abnormal cleavage of a transmembrane precursor protein and constitutes the neuropathological basis of Alzheimer’s disease29, along with the neurofibrillary tangles (protein aggregates of hyperphosphorylated tau protein). The vascular damage observed in almost 90 % of the brains of patients with Alzheimer’s disease contributes to the progress of the neurodegenerative process which, in turn, leads to its clinical expression (dementia), supporting the hypothesis that vascular and neurodegenerative injuries are the extreme points of a spectrum, within which most of the various forms of dementia can be found.
Neurodegenerative pathology seems to be a necessary but not sufficient condition. The vascular damage (endothelial dysfunction, ischaemia, blood-brain barrier disruption) alters the balance between A production and clearance, thus increasing A levels in the brain with the toxic consequences (reactive oxygen species production and inflammatory response)30.
Recent publications report that patients with treated but uncontrolled hypertension increase their brain A depositions31,32,33. Knowledge of the role vascular injury plays in the clinical expression of Alzheimer’s disease may open up new avenues to explore in the search for dementia prevention by employing strategies that either treat or prevent the vascular cause.