2) Orthostatic Hypotension
OH is defined as a reduction in systolic BP of at least 20 mmHg or in diastolic BP of at least 10 mmHg within 3 minutes of standing.60 Orthostatic intolerance (OI) refers to symptoms and signs with upright posture due to circulatory abnormality.1 Syndromes of OI that may cause syncope as per ESC guidelines include: initial OH where symptoms of lightheadedness/dizziness or visual disturbance are experienced seconds after standing; classic OH where dizziness, pre-syncope, fatigue, weakness, palpitations, visual and hearing disturbances are experienced; delayed OH where there is a prolonged prodrome frequently followed by rapid syncope; delayed OH and reflex syncope where there is a prolonged prodrome always followed by syncope; reflex syncope triggered by standing where there is classic prodrome and triggers always followed by syncope and postural orthostatic tachycardia syndrome where there is symptomatic HR increases and instability of BP without syncope.1 Many older patients with OH also have postprandial hypotension.
Prevalence of OH in the older-aged community-dwelling adults is 30 %61 and increases to more than 50 % in geriatric ward patients62 making its diagnosis highly relevant. Causes of OH include volume depletion or disturbance of the autonomic nervous system resulting in failure in vasoconstrictor compensatory mechanisms induced by upright posture.63 The prevalence is higher if phasic BP measures are used. In the TILDA population, 50 % of people over 70 years had persistent OH up to 40 seconds after standing. Failure of BP to return to baseline values is associated with adverse physical and cognitive outcomes such as syncope, falls, depression and cognitive dysfunction (Finucane, Impaired Orthostatic Blood Pressure Recovery is Independently Associated with an Increased Risk of Falls in Older Community Dwelling Adults; submitted).
The TILDA study has also shown that supine systolic hypertension (SSH) coupled with OH is a risk factor for cognitive impairment and depression.64 There is a striking age gradient in impaired orthostatic BP response as evidenced in Figure 4 (Finucane et al., Age related normative changes in phasic orthostatic blood pressure and prevalence of impaired recovery in a large population study: Findings from the Irish Longitudinal Study on Ageing (TILDA) – submitted to Circulation).
Causes of Orthostatic Hypotension
The following are the most common causes of OH in elderly people:
Differential diagnosis must also include anaemia and diagnosis of its underlying cause, Addison’s disease or malignancy.
Medication-induced Orthostatic Hypotension
Syncope due to OH is linked to the use of vasoactive medications, most commonly diuretics and nitrates.63 Many medications cause OH: cardiovascular medications such as alpha-blockers, diuretics, nitrates, neurological medications, anti-parkinsonian, anti-depressant medications and benzodiazepines.28,60,65 Multivariate analysis in one recent study found that predictors of OH were varicose veins and treatment with alpha-receptor blockers, nitrates or benzodiazepines.28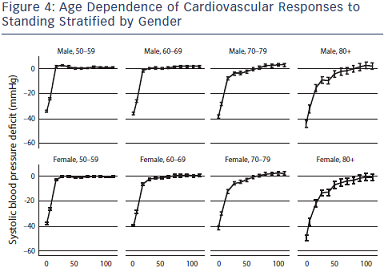
Investigation of Orthostatic Hypotension
Active standing or passive and unprovoked HUT resulting in symptoms coinciding with a 20 mmHg systolic or diastolic BP drop of 10 mmHg within 3 minutes of orthostatic stress confirms a diagnosis of OH.60 BP and HR usually recover to baseline values within 30 seconds but this reflex increase changes with age and haemodynamic recovery is delayed in elders (see Figure 4, Finucane et al.)
Ambulatory BP monitoring in OH patients guides assessment of diurnal variation in BP,1 postprandial hypotension, response to timing of medications and nocturnal supine hypertension.
Management of Orthostatic Hypotension
Culprit medications should be modified or eliminated and conservative measures adopted prior to consideration of additional pharmacotherapy.66 Conservative measures include PCM,67 enhanced fluid and salt intake, elevation of the head of bed when sleeping (modifies neuroendocrine control of nocturnal polyuria, redistribution of body fluids and supine hypertension),68,69 compression stockings, abdominal binders70,71 and rapid ingestion of cool water for symptoms of OI and post-prandial hypotension.72
Medications, such as midodrine (an alpha 1 agonist)73–75 and fludrocortisone (a mineralocorticoid that stimulates renal sodium retention and expands intravascular volume), are both well tolerated in the older patient in moderate dosages.68 Pyridostigmine, octreotide and desmopressin are adjunct therapies but are less well researched in older patients and less well tolerated in our experience.
The combination of SSH and OH poses challenging management decisions as treatment of SSH may worsen symptoms of OH.76 Attention to symptom relief is balanced with treatment of vascular risk associated with SSH.77,78 TILDA researchers reported that beta blockers and anti-depressants were risk factors for OH in people over 50 with SSH.78 Other cardiovascular medications were not associated with OH in people with SSH.