3) Cardiac Syncope
One-third of cases of syncope in the older patient are caused by cardiac disorders18 (see Figure 3).21 There is a higher morbidity and mortality associated with cardiac syncope.15,79 Cardiac syncope is characterised by little or no prodrome, occurrence when supine or during exercise and association with palpitations or chest pain.7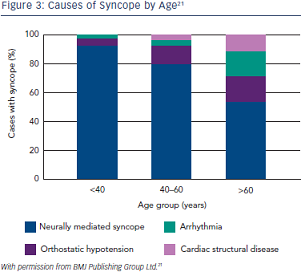 However, the older patient may not recall these symptoms. Heart disease is an independent predictor of cardiac syncope – sensitivity 95 % and specificity 45 %;80 the prevalence of cardiac disease, including structural heart disease and arrhythmias, rises dramatically with age as detailed in Figures 2 and 3.20,21,81 Cardiac syncope should be considered when the surface ECG is abnormal or left ventricular systolic dysfunction is present.7
However, the older patient may not recall these symptoms. Heart disease is an independent predictor of cardiac syncope – sensitivity 95 % and specificity 45 %;80 the prevalence of cardiac disease, including structural heart disease and arrhythmias, rises dramatically with age as detailed in Figures 2 and 3.20,21,81 Cardiac syncope should be considered when the surface ECG is abnormal or left ventricular systolic dysfunction is present.7
Investigation
The gold standard for the diagnosis of cardiac syncope is symptomrhythm correlation i.e. contemporaneous HR and rhythm recording during syncope. Cardiac monitoring may also identify diagnostic abnormalities, such as asystole in excess of 3 seconds and rapid supraventricular (SVT) or ventricular tachycardia (VT).82–84 The absence of an arrhythmia during a recorded syncopal event excludes arrhythmia as a cause unless the patient has a dual diagnosis. In patients over 40 years with recurrent unexplained syncope who do not have structural heart disease or abnormal ECG, the attributable cause of syncope is bradycardia in over 50 %.44,85–87
Cardiac Monitoring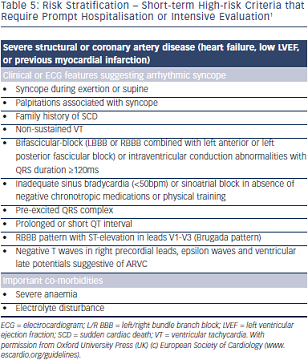
Prompt hospital admission or intensive monitoring is recommended when cardiac disease is present in the setting of syncope (see Table 5).1 Although telemetry or in-patient monitoring is indicated if the patient is at high risk of a life-threatening arrhythmia as per ECG abnormalities detailed in Table 5, the diagnostic yield from telemetry is low –16 % in one series.88 Holter monitoring is only indicated if a patient is experiencing episodes of sufficient frequency to detect an abnormality up to 72 hours of recording.1 Diagnostic yield from Holter monitoring is only 1–2 % in unselected populations.1 Incidental arrhythmias are much more common in older persons, for example, atrial fibrillation occurs in one in five men over 80 years.89
External loop recorders have a higher diagnostic yield in older patients; however, some older patients may have difficulty operating the devices,90,91 therefore automated arrhythmia detection is preferred.92 Normal ambulatory ECG (Holter or external loop or otherwise) in the absence of symptoms does not exclude a causal arrhythmia7 and monitoring for longer intervals is imperative to capture rhythm during symptoms.
Diagnostic rates are much higher in older patients using the ILR,93,94 up to 50 % in patients with syncope and unexplained falls.9,10,95 Early insertion of ILRs in the older person is important to consider in view of the disproportionately high number of cardiac causes of syncope in this group.9 This approach is also more cost-effective.96,97 Difficulties with ILRs include inability to activate the device, particularly if patients have cognitive impairment, however, automated recordings and remote monitoring have much improved diagnostic yield.42 Magnetic resonance imaging (MRI) brain scans are increasingly used for investigation of other symptoms in elderly persons, therefore, MRI compatible devices should always be used.
Echocardiography
Echocardiography (ECHO) should be performed in syncope patients in whom a structural abnormality is suspected. The prevalence of structural cardiac abnormalities increases with age.81 The test is of most benefit in older patients with aortic stenosis98 and to evaluate ejection fraction. Cardiac arrhythmias are evident in up to 50 % of patients with an ejection fraction of less than 40 %.99
Ambulatory Blood Pressure Monitoring
Patterns of BP behaviour including post-prandial hypotension, hypotension after medication ingestion, orthostatic and exerciseinduced hypotension and SSH can be readily identified by this investigation. Modification of timing of meals and medications is guided by BP patterns.24,100
Exercise Stress Testing
Exercise stress testing is indicated to investigate cardiac disease and in patients who present with exercise-induced syncope.1 It is not always possible in older patients who may alternatively require angiography to investigate cardiac status.
Electrophysiological Study
Electrophysiological study is indicated in the older non-frail patient with syncope when a cardiac arrhythmia is suspected.24 Diagnosis is based on confirmation of an inducible arrhythmia or conduction disturbance.101 The benefit is dependent on pretest probability based on the presence of organic heart disease or an abnormal ECG.102
Electrophysiological study has the advantage of providing both diagnosis and treatment in the same session (i.e. transcatheter ablation).24 It is most effective for identification of sinus node dysfunction in the presence of significant sinus bradycardia of 50 bpm or less; prediction of impending high-degree atrioventricular (AV) block in patients with bifascicular block; inducible monomorphic VT (in patients with previous myocardial infarction [MI]) and inducible SVT with hypotension in patients with palpitations.24
Management of Cardiac Syncope
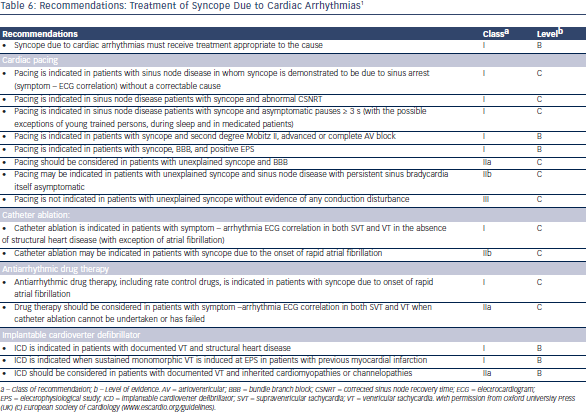
Management of cardiac syncope is dependent on specific cardiac diagnosis as outlined in see Table 6.1