Digoxin and Other Digitalis Glycosides
A central deficit in patients with HF is that in cardiac myocytes, calcium ions (Ca2+) handling is impaired, which is a causal factor for contractile dysfunction.52 A classical treatment of patients with HF is the use of digitalis glycosides, which inhibit the Na+/K+ adenosine triphosphatase (ATPase) and thus, elevate intracellular Na+ concentrations. This, in turn, increases Ca2+ influx via the Na+/Ca2+ exchanger, which increases cardiac contractility. As a second effect, digitalis glycosides prolong the refractoriness of the atrioventricular (AV)-node, which accounts for negative chronotropic effects in patients with AF, but less in SR (contrary to ivabradine). 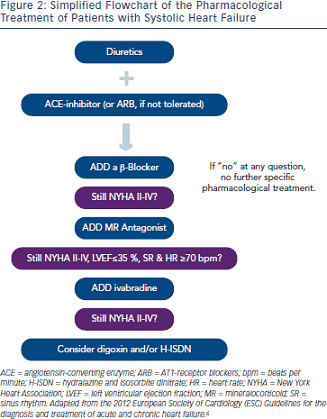 The only large randomised placebo-controlled trial with a glycoside was the Digitalis Investigation Group (DIG) trial,53 in which digoxin was compared with placebo in 6,800 patients in NYHA functional classes II-IV and a LVEF ≤45 %, added to a diuretic and an ACE-inhibitor. Published in 1997, this trial was before the time when β-blockers were widely used in patients with HF. The main outcomes of this trial were that digoxin reduced hospital admission for HF by 28 %, but did not affect all-cause mortality over three years.53
The only large randomised placebo-controlled trial with a glycoside was the Digitalis Investigation Group (DIG) trial,53 in which digoxin was compared with placebo in 6,800 patients in NYHA functional classes II-IV and a LVEF ≤45 %, added to a diuretic and an ACE-inhibitor. Published in 1997, this trial was before the time when β-blockers were widely used in patients with HF. The main outcomes of this trial were that digoxin reduced hospital admission for HF by 28 %, but did not affect all-cause mortality over three years.53
Combination of Hydralazine and Isosorbite Dinitrate
A characteristic hallmark in patients with HF is that through neuroendocrine activation, SVR is elevated, imposing an increased afterload to the failing heart. Thus, a therapeutic approach (that proved beneficial with ACE-inhibitors) is to lower SVR by applying vasodilating agents. Three trials investigated the effects of the vasodilatory combination of hydralazine and isosorbite dinitrate (H-ISDN) in patients with HF: first Vasodilator Heart Failure Trial (V-HeFT I),54 second Vasodilator-Heart Failure Trial (V-HeFT II)55 and African-American Heart Failure Trial (A-HeFT).56 In the Valsartan Heart Failure Trial (Val-HeFT I),54 H-ISDN increased exercise capacity and LVEF compared with placebo and showed a trend towards reduction in all-cause mortality.54 However, in that trial, no patient was treated with an ACE-inhibitor or a β-blocker. In V-HeFT II,55 H-ISDN was compared with the ACE-inhibitor enalapril, being inferior by tending to increase mortality by 28 % versus the ACE-inhibitor. A-HeFT compared H-ISDN to placebo added to a background medication including ACE-inhibitors or ARB (combined 84 %), digoxin (60 %), β-blockers (74 %) and spironolactone (39 %) exclusively in African- American patients with HF (NYHA III-IV).56 H-ISDN reduced mortality by 43 % and HF hospitalisation by 33 % and improved quality of life.56 Since results in white patients are currently inconclusive, the use of H-ISDN is recommended only for black patients and thus, uncommon in most European countries, while it is more common in the US.
Drugs Not Recommended
Despite its accepted benefit in patients with coronary artery disease, statins have not improved outcome in patients with HF. Rosuvastatin was neither efficient in patients with ischaemic nor non-ischaemic cardiomyopathy, based on the data of the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA)57 and the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico- Heart Failure (GISSI-HF) trial.58 Also, the renin inhibitor aliskiren was not efficient in decreasing rehospitalisation or cardiovascular death in patients with systolic HF.59 Drugs that could produce harm in patients with HF include thiazolidinediones (glitazones), calciumchannel blockers, non-steroidal anti-inflammatory drugs (NSAIDs) and cyclooxygenase-2 (COX-2) inhibitors and therefore should be avoided.6 Finally, the addition of an ARB to an ACE-inhibitor and a MRA is not recommended due to the risk of renal dysfunction and hyperkalaemia.6
Summary
Taken together, patients with HF should be treated with diuretics to prevent or treat symptoms of congestion, and with an ACE-inhibitor, β-blocker and MRA to improve morbidity and mortality. For some patients, the use of ivabradine or digoxin and/or H-ISDN may be useful. In Figure 2, a simplified scheme adapted from the current guidelines on the treatment of patients with chronic systolic HF is illustrated that helps to choose the right drugs at the right time in the treatment of these patients.
Christoph Maack is supported by the Deutsche Forschungsgemeinschaft (Heisenberg Programm, SFB 894) and the Deutsche Herzstiftung (Margret Elisabeth Strauß Projektförderung).