Valves
Currently, two main groups of artificial valves or prosthesis are available for aortic valve replacement. These are mechanical valves and tissue/bioprosthetic valves. The main advantage of mechanical valves is their excellent durability. Their principal disadvantage is the need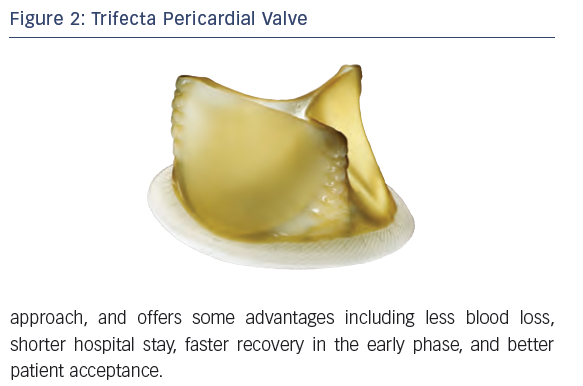 for lifelong anticoagulation therapy due to increased risk for blood clots. Tissue valves, on the other hand, have less durability and tend to wear out sooner than mechanical valves. However, they do not require lifelong anticoagulation. Over the last 2 decades, there has been a growing trend to implant more tissue aortic valves as opposed to mechanical valves.15 Tissue aortic valves (e.g. bovine, porcine, and homografts/human cadaveric aortic valves) can be stented or stentless. One major concern with stented (tissue mounted on a stent) bioprosthesis has been the less-than-optimal systolic hemodynamic performance with the smaller sizes. Stentless bioprosthesis have excellent hemodynamics but are generally more complex to implant in the subcoronary position or are carried out as a root replacement, which is a longer and more complex procedure. In this review, we will focus on the more commonly used stented bioprosthesis. TAVR series have shown excellent systolic hemodynamic function in all annular sizes thus presenting a challenge for sAVR using stented bioprosthesis.16,17 Valve innovation is fortunately still occurring and one answer to improving the systolic hemodynamics of the stented bioprosthesis is the new St Jude Medical Trifecta valve (St Paul, Minnesota, US).
for lifelong anticoagulation therapy due to increased risk for blood clots. Tissue valves, on the other hand, have less durability and tend to wear out sooner than mechanical valves. However, they do not require lifelong anticoagulation. Over the last 2 decades, there has been a growing trend to implant more tissue aortic valves as opposed to mechanical valves.15 Tissue aortic valves (e.g. bovine, porcine, and homografts/human cadaveric aortic valves) can be stented or stentless. One major concern with stented (tissue mounted on a stent) bioprosthesis has been the less-than-optimal systolic hemodynamic performance with the smaller sizes. Stentless bioprosthesis have excellent hemodynamics but are generally more complex to implant in the subcoronary position or are carried out as a root replacement, which is a longer and more complex procedure. In this review, we will focus on the more commonly used stented bioprosthesis. TAVR series have shown excellent systolic hemodynamic function in all annular sizes thus presenting a challenge for sAVR using stented bioprosthesis.16,17 Valve innovation is fortunately still occurring and one answer to improving the systolic hemodynamics of the stented bioprosthesis is the new St Jude Medical Trifecta valve (St Paul, Minnesota, US).
The Trifecta valve is an externally wrapped, stented pericardial valve designed to allow a larger effective orifice area (EOA) (see Figure 2). A clinical trial with this  valve was conducted from 2007 to 2009 at 31 centers and published in 2014.18 The question of poor hemodynamic performance in the smaller sizes did not appear in this series. All valves from 19 mm to 29 mm had single digit mean gradients at discharge. At 1 year, this still held true for all but the 19 mm size, which had a mean gradient of 10.7 mm Hg, which is still highly desirable. Mean indexed EOA at 1 month did not show any patient prosthetic mismatch (PPM) and only the 19 mm size gave an indexed EOA of 0.85 cm2/m2, which is the absolute upper end of moderate PPM. Early results with the Trifecta valve are promising, with indications of improved systolic hemodynamics and potential advantages of lower transvalvular gradients. However we would like to point out that, currently, this is one of the several options available and that longer term follow-up data are necessary to evaluate the effectiveness and durability of this design. Further, if this valve does undergo structural valve deterioration necessitating a new valve, the external pericardial wrap may make coronary occlusion a greater risk if the TAVR valve-in-valve method is chosen and this remains to be tested.
valve was conducted from 2007 to 2009 at 31 centers and published in 2014.18 The question of poor hemodynamic performance in the smaller sizes did not appear in this series. All valves from 19 mm to 29 mm had single digit mean gradients at discharge. At 1 year, this still held true for all but the 19 mm size, which had a mean gradient of 10.7 mm Hg, which is still highly desirable. Mean indexed EOA at 1 month did not show any patient prosthetic mismatch (PPM) and only the 19 mm size gave an indexed EOA of 0.85 cm2/m2, which is the absolute upper end of moderate PPM. Early results with the Trifecta valve are promising, with indications of improved systolic hemodynamics and potential advantages of lower transvalvular gradients. However we would like to point out that, currently, this is one of the several options available and that longer term follow-up data are necessary to evaluate the effectiveness and durability of this design. Further, if this valve does undergo structural valve deterioration necessitating a new valve, the external pericardial wrap may make coronary occlusion a greater risk if the TAVR valve-in-valve method is chosen and this remains to be tested.
Sutureless Valves
The concept of an aortic valve that could be placed without sutures is not new and in fact originated with the McGovern-Cromie valve in 1964 (see Figure 3). The success of TAVR has refocused attention in this area and currently three sutureless aortic valves are either available outside of the US or being tested here (see Figure 4). The 3f Enable bioprosthesis by Medtronic (Medtronic, Inc., Minneapolis, Minnesota, US) and 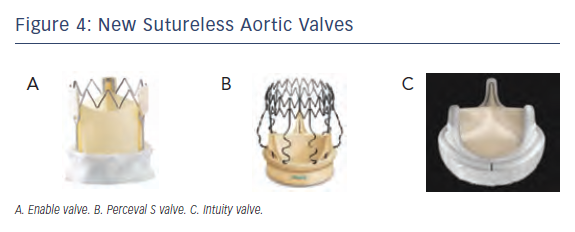 the Perceval S by Sorin (Sorin Biomedica Cardio Srl, Saluggia, Italy) are self-expanding with Nitinol frames and pericardial leaflets. The Intuity by Edwards (Edwards Lifesciences, Irvine, California, US) has a balloon-expandable frame and pericardial leaflets. Although termed sutureless valves, guiding sutures are often used to seat the valve properly and a better term for them might be rapid deployment valves. These valves are placed when the patient is on CPB with aortic cross-clamp (ACC) under cardioplegic arrest. The native stenotic leaflets are removed, but without the meticulous decalcification normally carried out for a sAVR, as some remaining calcium will help hold the valve in place. The concept for these valves is that they would simplify valve implantation by shortening both cross-clamp time and cardiopulmonary bypass times and maintain the excellent hemodynamics seen in TAVR, but with a decreased incidence of paravalvular leak (PVL), and thus will allow increased adoption of minimally invasive surgical approaches to sAVR. Shortening cross-clamp and CBP times is appealing in terms of reducing operative time and because these are known to carry the risk for postoperative mortality and morbidity, especially in higher risk patients, or when combined procedures need to be performed (AVR/coronary artery bypass surgery [CABG] or multiple valves).19
the Perceval S by Sorin (Sorin Biomedica Cardio Srl, Saluggia, Italy) are self-expanding with Nitinol frames and pericardial leaflets. The Intuity by Edwards (Edwards Lifesciences, Irvine, California, US) has a balloon-expandable frame and pericardial leaflets. Although termed sutureless valves, guiding sutures are often used to seat the valve properly and a better term for them might be rapid deployment valves. These valves are placed when the patient is on CPB with aortic cross-clamp (ACC) under cardioplegic arrest. The native stenotic leaflets are removed, but without the meticulous decalcification normally carried out for a sAVR, as some remaining calcium will help hold the valve in place. The concept for these valves is that they would simplify valve implantation by shortening both cross-clamp time and cardiopulmonary bypass times and maintain the excellent hemodynamics seen in TAVR, but with a decreased incidence of paravalvular leak (PVL), and thus will allow increased adoption of minimally invasive surgical approaches to sAVR. Shortening cross-clamp and CBP times is appealing in terms of reducing operative time and because these are known to carry the risk for postoperative mortality and morbidity, especially in higher risk patients, or when combined procedures need to be performed (AVR/coronary artery bypass surgery [CABG] or multiple valves).19
Sutureless aortic valves are still early in their development and a number of smaller trials with these exist. One of the larger trials was reported by Kocher and involved 146 patients in six European centers using the Intuity valve.20 The 1-year hemodynamic performance was good but two early and two late valve explants were required. The ACC time was 41.1 minutes and only 31.1 % of the cases were performed via a minimally invasive approach. A propensity matched study between 519 patients having TAVR or sAVR using the Perceval S valve and then matched to 38 pairs has been presented by D’Onofrio.21 Hemodynamic performance, complications, and pacemaker insertion rates were similar between the groups. Differences were seen in a greater rate of atrial fibrillation in the sAVR group (42 % versus 16 %) and a lesser rate of at least mild PVL in the sAVR group (16 % versus 45 %), though PVL results along the same lines may not be representative of all studies. Current data on sutureless aortic valves would suggest that they can be used safely, with good hemodynamics and with acceptable complication rates. It is however unknown if this will increase the adoption of minimally invasive approaches to sAVR or improve patient outcomes. Also unknown is the long-term durability of these valves. Despite these areas of concern, these valves offer the potential for a simplified and reproducible technique for sAVR, provide another tool in the toolbox of aortic surgeons, and deserve further study.