Aortic Valve Repair
The success of mitral valve repair in treating mitral regurgitation has prompted the development of repair techniques for aortic regurgitation. Successful aortic valve repair as opposed to sAVR would allow the patient to avoid anticoagulation as well as structural valve  deterioration. Successful aortic valve repair, like mitral valve repair, requires an understanding of the mechanisms leading to aortic insufficiency (AI). A functional classification of AI similar to the Carpentier classification for mitral regurgitation has been presented by El Khoury22 (see Figure 5). Type I AI shows central regurgitation. This can occur from dilatation of the annulus or the sinotubular junction. Dilatation of the sinuses alone does not lead to AI. Additionally a perforation of the valve cusp can lead to a Type I central regurgitation. An eccentric regurgitation from cusp prolapse is seen in Type II and from cusp restriction in Type III. Repair techniques, as with mitral valve repair, are dependent on the mechanism causing the regurgitation.
deterioration. Successful aortic valve repair, like mitral valve repair, requires an understanding of the mechanisms leading to aortic insufficiency (AI). A functional classification of AI similar to the Carpentier classification for mitral regurgitation has been presented by El Khoury22 (see Figure 5). Type I AI shows central regurgitation. This can occur from dilatation of the annulus or the sinotubular junction. Dilatation of the sinuses alone does not lead to AI. Additionally a perforation of the valve cusp can lead to a Type I central regurgitation. An eccentric regurgitation from cusp prolapse is seen in Type II and from cusp restriction in Type III. Repair techniques, as with mitral valve repair, are dependent on the mechanism causing the regurgitation.
Type I Aortic Regurgitation
Central regurgitation due to cusp perforation can occur in endocarditis or trauma. If the regurgitation is limited, it can be repaired by pericardial patch closure. The more common causes of Type I AI are annular and sinotubular junction dilatation. Occasionally, the AI is due to dilatation of the sinotubular junction when an ascending aortic aneurysm is the only pathology. The aortic aneurysm can be repaired by graft replacement of the ascending aorta. The diameter of the graph is 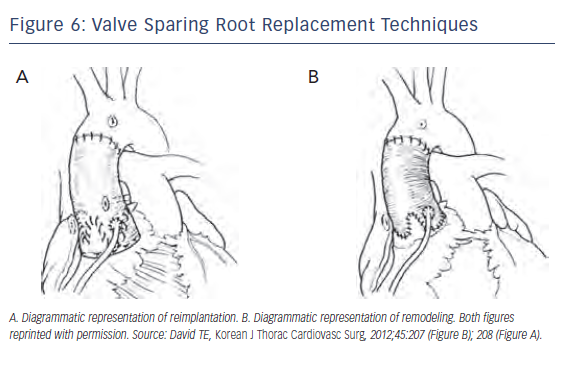 equal to the free margin (annular diameter) of the cusps or slightly undersized. This brings the commissural posts back into alignment and allows proper coaptation of the valve cusps to eliminate AI. Annular dilatation requires reducing the annular diameter. Although there are subannular rings being developed for this purpose similar to mitral rings, they are still early in their development. This is more commonly performed using a valve sparing root replacement (VSRR) technique. Two common approaches have been used for fixing annular dilatation: remodeling introduced by Sarsam et al.23 and the reimplantation technique introduced by David et al.24
(see Figure 6) The remodeling technique removes the sinuses and coronaries are freed up as buttons, leaving the aortic valve and a several millimeter rim of sinus above the annulus. A graft is then fashioned with tongues that extend down to replace the sinuses and the coronary buttons are then reimplanted. The reimplantation technique differs in that the graft is brought over the remaining valve and rim of the sinus tissue. The graft is loosely sewn with subannular sutures extending out through the graft to hold it in place. The valve complex is then sewn inside the graft forming the hemostatic sealing suture line. The coronaries are then reimplanted in a standard fashion. The reimplantation technique allows stabilization of the annulus unlike remodeling. Reimplantation may potentially be a better approach for a patient subject to recurring annular dilatation like patients with connective tissue disorders or bicuspid valves.
equal to the free margin (annular diameter) of the cusps or slightly undersized. This brings the commissural posts back into alignment and allows proper coaptation of the valve cusps to eliminate AI. Annular dilatation requires reducing the annular diameter. Although there are subannular rings being developed for this purpose similar to mitral rings, they are still early in their development. This is more commonly performed using a valve sparing root replacement (VSRR) technique. Two common approaches have been used for fixing annular dilatation: remodeling introduced by Sarsam et al.23 and the reimplantation technique introduced by David et al.24
(see Figure 6) The remodeling technique removes the sinuses and coronaries are freed up as buttons, leaving the aortic valve and a several millimeter rim of sinus above the annulus. A graft is then fashioned with tongues that extend down to replace the sinuses and the coronary buttons are then reimplanted. The reimplantation technique differs in that the graft is brought over the remaining valve and rim of the sinus tissue. The graft is loosely sewn with subannular sutures extending out through the graft to hold it in place. The valve complex is then sewn inside the graft forming the hemostatic sealing suture line. The coronaries are then reimplanted in a standard fashion. The reimplantation technique allows stabilization of the annulus unlike remodeling. Reimplantation may potentially be a better approach for a patient subject to recurring annular dilatation like patients with connective tissue disorders or bicuspid valves.
Type II Aortic Regurgitation
Cusp prolapse may occur with Type I anatomy or in isolation. The base of the valve cusp is generally about 1.5 times longer than the free margin of the cusp. If the free margin elongates and approaches the length of the base, then the cusp will prolapse into the ventricle during diastole and allow AI. The surgical solution to this is to shorten the free margin length of the cusp. This can be performed by resection of the center point of the elongated cusp or just suture imbrication of this area. The cusps can also be shortened by imbrication at the aortic wall or by placing a free margin suture of fine polytetrafluoroethylene (PTFE).
Type III Aortic Regurgitation
Like restricted leaflets in mitral regurgitation, cuspal restriction in AI does not lend itself well to repair using current techniques and generally requires valve replacement.
Outcomes for Aortic Valve Repair and Valve Sparing Aortic Root Procedures
Long-term results have been reported for several studies that have used the remodeling or reimplantation approach. Following remodeling, freedom from moderate or severe AI at 10 years was 64 % in the study by Yacoub et al.,25 96 % for bicuspid valves, and 87 % for tricuspid valves as reported by Aicher et al.26 Following reimplantation, freedom from reoperation at 10 years was 93 % for David et al.27 and 88 % for De Paulis et al.28 Aortic valve sparing operations have been shown to have good long-term outcomes in experienced centers and offer the ability to maintain the patient’s native valve.