Mitral valve
Motivated by the success of TAVR, transcatheter mitral valve procedures are seen as the next frontier of structural cardiac interventions for patients at high surgical risk. These procedures consist in the implantation of a device that repairs or replaces the native mitral valve leaflets with the goal of reducing mitral valve regurgitation. The therapies fall into four categories49; edge-to-edge repair (MitraClip), annuloplasty rings (Carillon, Mitralign, Accucinch, Cardioband), chordal implants (NeoCho rd, V-Chordal) and transcatheter mitral valve replacement (CardiAQ mitral valve, Fortis mitral valve, TIARA mitral valve, Tendyne mitral valve, HighLife mitral valve). These therapies are at various stages of development, from pre-clinical research to commercial availability.
rd, V-Chordal) and transcatheter mitral valve replacement (CardiAQ mitral valve, Fortis mitral valve, TIARA mitral valve, Tendyne mitral valve, HighLife mitral valve). These therapies are at various stages of development, from pre-clinical research to commercial availability.
MSCT will likely play a crucial goal in the assessment of the mitral valvular complex with these new therapies. MSCT has been investigated to assess the function and anatomy of the mitral valve. In the context of mitral regurgitation, MSCT can be used to determine the disease etiology,50,51 to quantify the severity,52,53 to describe changes in the geometry of the valvular complex54,55 and to diagnose mitral valve prolapse.56–58
In the context of transcatheter mitral valve replacement (TMVR), MSCT has been proposed to quantify the mitral valve annulus. The mitral valve annulus is often described as either saddle-shaped or as D-shaped (see Figure 6). It has been argued that for some of the devices, in particular those that are not axially symmetrical, the D-shaped annulus may be more appropriate for sizing purposes.59,60 This question remains to be studied, but in the interim we suggest that both techniques be 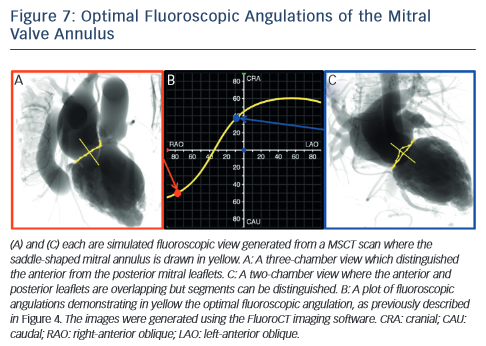 employed.
employed.
MSCT also plays a role in the optimisation of fluoroscopic viewing angles for mitral valve therapies.31,61 In particular, MSCT allows one to determine the optimal projection curve of the mitral valve annulus (see Figure 7). One may also preselect a fluoroscopic viewing angle corresponding to two-chamber view, which distinguishes mitral valve segments A1P1 from A2P2 and from A3P3 but overlaps the anterior and posterior leaflets such that A1 overlaps P1, A2 overlaps P2, and A3 overlaps P3. Conversely, one may preselect a fluoroscopic viewing angle corresponding to a three-chamber view that distinguishes the ante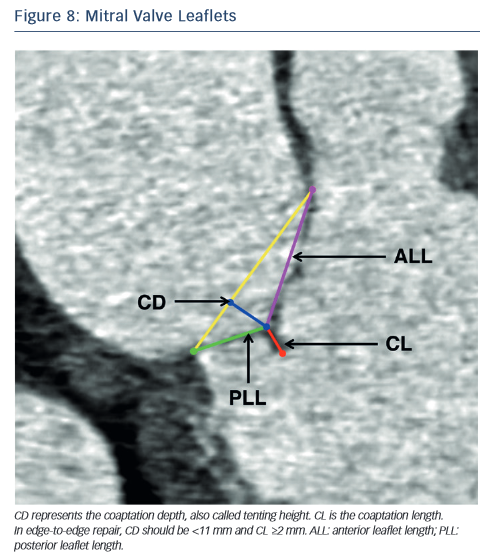 rior from the posterior leaflets but overlaps segments A1,2,3 and separately P1,2,3.
rior from the posterior leaflets but overlaps segments A1,2,3 and separately P1,2,3.
In the context of percutaneous edge-to-edge repair such as the MitraClip procedure, MSCT has been proposed for patient selection. Anatomical criteria essential for this procedure include:62,63 (1) central regurgitant jet located in the A2 and P2 mitral leaflets; (2) in functional mitral regurgitation, a coaptation length ≥2 mm and coaptation depth <11 mm (see Figure 8) and (3) in degenerative mitral regurgitation, a flail gap <10 mm and flail width <15 mm.
As new mitral valve devices undergo clinical trials, MSCT will likely play a critical role in determining patient eligibility. Further research is necessary to determine if MSCT has an impact on procedural success and clinical outcomes of these interventions.