Thromboembolic Prophylaxis by Left Atrial Appendage Closure
Atrial fibrillation (AF) is the most common arrhythmia in the general population76 and is an important factor in the pathophysiology of atrial thrombus formation. Chronic anticoagulation is gene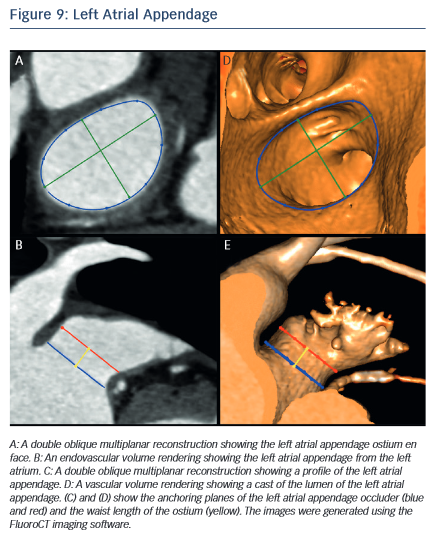 rally indicated in patients with AF and deemed at risk for stroke. A significant number of patients for whom thromboprophylaxis would be indicated are not eligible due to a high bleeding risk. Interestingly, studies suggest that 90 % of thrombus causing strokes in patients with AF originate from the left atrial appendage (LAA).77 This is thought to result from the presence of pectinate muscles within the LAA thus creating an appropriate milieu for blood stasis and thrombus formation. This prompted the development of surgical LAA ligation and eventually, of minimally invasive procedures.
rally indicated in patients with AF and deemed at risk for stroke. A significant number of patients for whom thromboprophylaxis would be indicated are not eligible due to a high bleeding risk. Interestingly, studies suggest that 90 % of thrombus causing strokes in patients with AF originate from the left atrial appendage (LAA).77 This is thought to result from the presence of pectinate muscles within the LAA thus creating an appropriate milieu for blood stasis and thrombus formation. This prompted the development of surgical LAA ligation and eventually, of minimally invasive procedures.
Percutaneous transcatheter LAA closure was first described in 2002 and has since been studied in clinical trials. The Watchman Left Atrial Appendage System for Embolic Protection in Patients With Atrial Fibrillation trial (PROTECT AF trial) demonstrated that the procedure is non-inferior to warfarin therapy but resulted in higher rates of complications such as pericardial effusion.78 Four devices are currently available or under investigation: the WATCHMAN device, the Amplatzer Cardiac Plug, the WaveCrest device and the Lariat epicardial suturesnare delivery device.
MSCT allows the anatomy of the LAA to be evaluated, which is valuable for device selection,79 assessment of procedural success and longer-term outcomes.80 It has been suggested that the perimeter-derived diameter of the LAA ostium is the most appropriate for device sizing.79 Other important parameters include the minimum and maximum diameters, as well as the waist length of the LAA ostium81 (see Figure 9). MSCT can also be used to determine optimal fluoroscopic angulation for the deployment of the LAA closure device.31
The information provided by MSCT regarding outcomes is complementary to that obtained from transoesophageal echocardiography (TEE). MSCT has a higher rate of detection than TEE for device leaks, which are defined as flow of blood within the LAA past the device.82 The localisation of leaks is also easier with MSCT than with TEE.82 Contrast-enhanced MSCT also enables the evaluation of device thrombus,83 embolisation and pericardial effusion.84,85 Further studies are necessary to provide evidence regarding the impact of MSCT imaging on outcomes of LAA closure.