Paravalvular Leak: Imaging
Successful PVL closure begins with efficient imaging. There are a variety of methods available to diagnose PVL, including transthoracic echocardiography (TTE), transoesophageal echocardiography (TEE), computerised tomography (CT) and magnetic resonance imaging (MRI). Among these, there is no one optimal diagnostic method; each has significant advantages and disadvantages. The important pieces of information to ascertain during imaging are location, size, shape, severity and the number of leaks.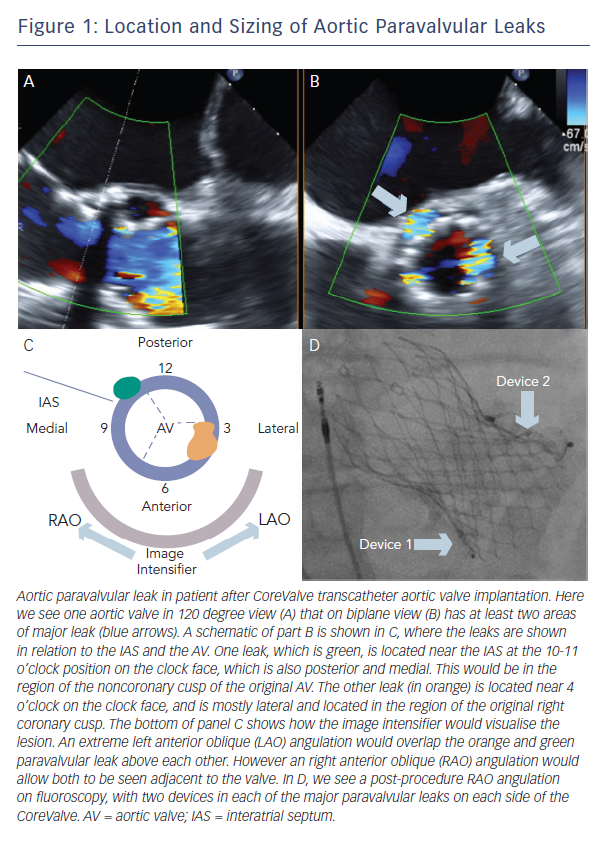
It is important to know the valve type prior to any imaging (often available from the surgical report), and it can also be helpful to know its orientation and the suturing technique that was used. Orientation of the valve varies, but often the preferred mitral orientation for tilting-disc valves is with the major orifice toward the left ventricular free wall as opposed to the septum. For the aortic position, the preferred orientation is with the major orifice to the right posterior aortic wall. Suturing techniques may also vary, ranging from non-everting mattress (with or without sub-annular pledgets), everting mattress (with or without supra-annular pledgets), simple interrupted, figure-of-eight, and continuous/running sutures. The choice of suture technique depends on valve type and surgeon preference.
Echocardiography allows for direct comparison of pre- and intra-procedural results. However, echocardiography is prone to artifact from prosthetic shadowing.7 Aortic PVL can be diagnosed and evaluated often by TTE, whereas mitral PVL often requires TEE (although TTE may be useful for original diagnosis). 3D echocardiography adds the ability to determine the path of a leak, which can often take a serpentine course. The authors perform all PVL interventions with TEE guidance (often with 3D characterisation of leak size and course).
CT and MRI add further information. Retrospective ECG-gated reconstruction allows diastolic and systolic characterisation. CT can also provide the accurate imaging angle for intervention and closure.Unfortunately, artifacts secondary to calcification or the valve can blur the leak itself, making it difficult to visualise. CT, in comparison to MRI, has better spatial resolution, however requires contrast dye and involves exposures to more radiation.8
Location
A clock face is often used to describe both aortic and mitral PVLs (Figure 1, Figure 2). The three commissures are assigned an hour on the clock face: between left and right coronary sinus is 5 o’clock, between right and non-coronary sinus is 8 o’clock, non-coronary and left coronary sinus is 11 o’clock. This lexicon helps in communication between imager and operator and also helps to monitor leaks pre- and post-closure. Statistically, aortic leaks are most often between 7 and 11 o’clock (46 %) and also between 11 and 3 o’clock (36 %). 9
Both clock face and anatomical criteria can be used to describe mitral PVL location. Location is based on the mitral valve annulus and is described as medial, lateral, anterior or posterior. The clock face for the mitral valve starts at the 12 o’clock position between the aortic valve and mitral valve A2, then the 3 o’clock position is the posteromedial commissure and interatrial septum and the 6 o’clock position is the posterior annulus midpoint. According to this system, mitral PVL is found often between 10 and 2 o’clock (45 %) and between 6 and 7 o’clock (37 %).9
Sizing
Although the course of the leak may be serpentine, with an orifice that is crescentic or oval in shape, some assumptions can be made about size of the PVL. Echocardiography of the vena contracta of the leak can be used to estimate the size, although this method is not perfect. With the advent of 3D imaging, the leak can be measured in multiple directions. CT and MRI may provide more information if an echocardiogram is unclear. The authors do not recommend balloon sizing as it is associated with a risk of balloon rupture as a consequence of sharp edges due to annular calcium. Measurement of the leak will dictate the choice of device for PVL access, and in turn the delivery system guide or sheath size.