OPTISTM Integrated System – A New OCT Imaging System with Online Angiographic Co-registration
The OPTISTM integrated system (St. Jude Medical, St Paul, MN, US) is an OCT imaging system that is integrated in the catheterisation laboratory and has the additional ability to provide a real-time co-registration of OCT images with the angiogram of the studied vessel. The OPTIS integrated system can be directly installed in a catheterisation laboratory and consists of the OCT imaging system, a pullback device, monitors and a tableside controller, while image acquisition is being performed with the DragonflyTM Duo (St. Jude Medical) OCT imaging catheter.
The imaging system is located within the control room of the catheterisation laboratory, while OCT data are projected in real time on a screen within the intervention room. Angiographic data from the existing angiographic system are retrieved and displayed simultaneously on the same screen. The pullback device is stowed in a holster positioned at the cath lab table. Direct tableside controls at the cath lab table allow for an autonomous handling of the system by the operating physician without the need for extra cable connections as in systems based on mobile carts. The OCT system specifications are similar to the previously used ILUMIENTM OPTISTM PCI Optimization system (St. Jude Medical) allowing for acquisition of OCT images with a frame rate of 180 frames per second. The pullback speed can be adjusted by the operator in one of two settings:
The Dragonfly Duo imaging catheter is a 2.7 F, rapid exchange monorail catheter with a pullback speed up to 75 mm/sec. Further, the distal catheter end carries a number of markers: a distal radiopaque marker indicating the guidewire exit, a proximal marker that indicates the ending position of the pullback and a marker indicating the position of the OCT lens. This marker moves simultaneously with the lens and allows the real-time tracking of its position by fluoroscopy. Finally, a femoral shaft guide marker has been added to identify when the Dragonfly Duo catheter is exiting a 100 cm guide catheter.
A number of options for displaying the OCT information are available. These include an automated lumen profile, which is generated after automated lumen detection in all OCT cross-sectional images throughout the pullback. This view provides information regarding the mean luminal diameter along the pullback, thus enabling a luminographic assessment of the studied vessel, but with the use of OCT measurements, overcoming potential limitations of angiography in luminal assessment such as foreshortening, vessel overlap or filling artifacts.
Information such as minimal lumen diameter, reference diameters and degree of area or diameter st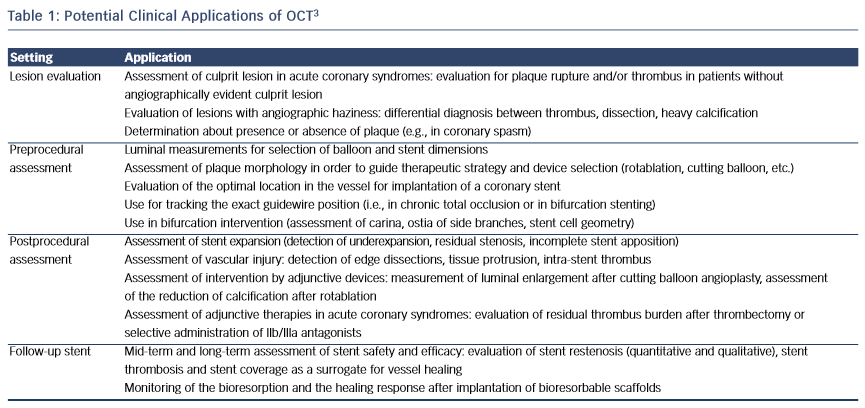 enosis are simultaneously projected on the screen, thus providing a fast and practical assessment of the severity of luminal stenosis, while giving important information for sizing. Moreover, OCT information is also reconstructed in 3D and can be displayed in parallel. This visualisation might aid in the assessment of bifurcations or in cases with stent deformation.
enosis are simultaneously projected on the screen, thus providing a fast and practical assessment of the severity of luminal stenosis, while giving important information for sizing. Moreover, OCT information is also reconstructed in 3D and can be displayed in parallel. This visualisation might aid in the assessment of bifurcations or in cases with stent deformation.
The angiographic image that is recorded during the pullback is projected together with the OCT image. After semi-automatic co-registration, a small white marker is projected over the angiogram, indicating the exact location of the displayed OCT frame on the angiogram. This information is useful for the direct utilisation of intravascular imaging findings in procedural decision making, as the location of the OCT images is directly displayed and facilitates the selection of a suitable landing zone for the intervention.
Clinical Relevance of Online OCT Co-registration
Overall, the use of a system able to provide online spatial co-registration of the high-resolution intravascular imaging findings with the angiographic image could improve decision-making in the cath lab. This integration of OCT information on an angiographic roadmap enables the easy and immediate utilisation of such information by the operator. This could find broad application in the treatment of complex or diffuse disease, where spatial orientation might be challenging, requiring continuous fluoroscopy and multiple views in order to correctly localise the segment that needs to be treated.
The advantage of using a co-registered OCT approach might be even more pronounced in the case of bioresorbable scaffold implantation. As the current designs of bioresorbable scaffolds have relatively thick struts and high crossing profiles, an extensive lesion preparation is required in order to be able to advance the device to the site of the lesion and achieve an optimal implantation result. An accurate delineation of the required landing zone is mandatory in order to avoid problems such as a mismatch between lumen scaffold dimensions or incomplete lesion coverage. Mismatch of lumen and scaffold dimensions should be avoided considering the narrow postdilation limits of bioresorbable scaffolds, where expansion above the recommended limits has been associated with fracture.8 Furthermore, in view of the need for extended vessel preparation with increased incidence of predilation, vessel injury might be more pronounced in comparison with metallic devices, where direct implantation is usually preferred. This has important clinical implications, as incomplete lesion coverage has been associated with bioresorbable scaffold failure.9,10 Therefore, a complete coverage by the scaffold of the segment subjected to predilation is desired, and the co-registration of the angiogram with OCT images providing information regarding the injured and healthy vessel wall can aid in ensuring this optimal coverage.
Another important field where OCT can provide useful guidance in clinical practice is in the management of stent failure, where the recent European Society of Cardiology guidelines have given OCT a class IIa recommendation (level of evidence: C).11 In acute and subacute stent thrombosis, mechanical factors such as incomplete expansion and vessel trauma play a pivotal role.5 It is important to recognise these mechanical complications in order to provide the appropriate treatment (e.g., postdilation in incomplete expansion or additional stent implantation in edge injury). The knowledge of the precise anatomical location can facilitate local treatment, especially in long stents or stents with asymmetric expansion, where the exact localisation of the site with the mechanical issue might be poorly visualised by angiography. Also, in late stent failure, the distinction of restenosis with thrombosis might be unclear by angiography,12 while use of OCT can help discriminate between these two mechanisms, and guide the choice between local or systematic antithrombotic therapy, balloon postdilation or additional stent implantation. Again, the localisation of the stent pathology is important, as the severity and extent of restenotic tissue and/or thrombus could vary, while the visualisation by the angiography remains poor. In such cases, co-registered OCT could allow treatment that is focused on treating the proper segment within the stent.
Overall, in our practice, OCT is being frequently used in the preprocedural lesion assessment providing accurate measurements for stent or scaffold sizing, aiding in the choice of the interventional strategy and in the delineation of a suitable landing zone. According to our experience, the use of a co-registered OCT system often facilitates decision making in a way readily and easily available, without obstructing the workflow of the laboratory. The integration of structural OCT information into the angiographic luminogram provides the desired angiographic landmarks that indicate the desired segment for positioning of the stent or the balloon. This finds application also for the postprocedural assessment where co-registration has proved to be useful in precisely localising regions with marked malapposition or incomplete expansion and treating appropriately. This strategy can help ensure an optimal implantation result, with adequate device expansion and apposition and minimisation of vessel injury. The following cases describe how co-registered OCT can be used in daily practice to improve outcomes.
The publication of this information was supported by St. Jude Medical.