Case study 1. OCT-guided BVS Implantation in a Patient with Acute Coronary Syndrome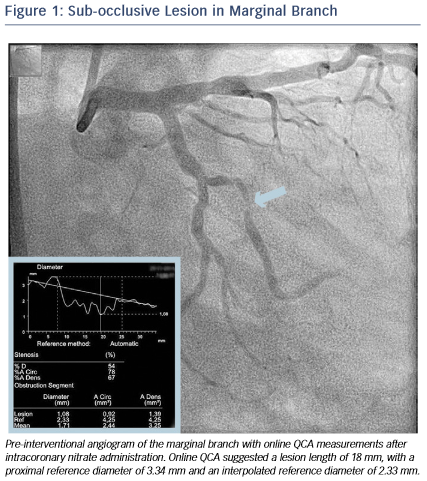
A 46-year-old male without cardiovascular history underwent coronary catheterisation for non-ST elevated myocardial infarction. Angiogram showed a sub-occlusive lesion in the marginal branch that was considered the culprit (see Figure 1), with an online measured interpolated reference diameter of 2.33 mm by Quantitative Coronary Angiography (QCA), while the lesion length was 18 mm.
After predilation with a 2.5 x 15 mm balloon, an OCT pullback co-registered with the angiogram was acquired in 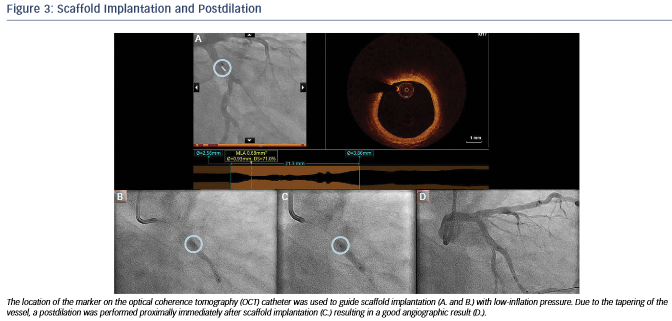 order to assess the lesion, select device size and determine the landing zone. Cross-sectional OCT images (see Figure 2) revealed an occlusive lesion at the minimal lumen area. At the angiographically suggested proximal reference segment, OCT revealed the presence of a thin- cap fibroatheroma with mural thrombus. Therefore, another more proximal landing zone was selected based on the OCT images, with a mean diameter of 3.86 mm and a maximum diameter of 3.93 mm. As the maximum diameter in the proximal landing zone was below 4 mm, we selected a 3.5 mm AbsorbTM (Abbott Vascular, Santa Clara, CA, US) bioresorbable scaffold that can be safely expanded up to a 4 mm diameter. Also, seeing the high-risk plaque morphology at the angiography su
order to assess the lesion, select device size and determine the landing zone. Cross-sectional OCT images (see Figure 2) revealed an occlusive lesion at the minimal lumen area. At the angiographically suggested proximal reference segment, OCT revealed the presence of a thin- cap fibroatheroma with mural thrombus. Therefore, another more proximal landing zone was selected based on the OCT images, with a mean diameter of 3.86 mm and a maximum diameter of 3.93 mm. As the maximum diameter in the proximal landing zone was below 4 mm, we selected a 3.5 mm AbsorbTM (Abbott Vascular, Santa Clara, CA, US) bioresorbable scaffold that can be safely expanded up to a 4 mm diameter. Also, seeing the high-risk plaque morphology at the angiography su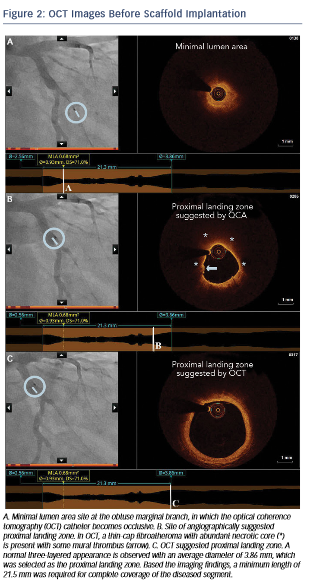 ggested landing zone, a 23 mm long scaffold was selected instead of the 18 mm suggested by angiography for complete coverage of the diseased segment. Furthermore, we decided upfront that postdilatation would be necessary in order to match the proximal reference diameter. A 3.5 x 23 mm scaffold was then implanted with low-pressure inflation in order to avoid vessel injury due to the tapering of the vessel distally.
ggested landing zone, a 23 mm long scaffold was selected instead of the 18 mm suggested by angiography for complete coverage of the diseased segment. Furthermore, we decided upfront that postdilatation would be necessary in order to match the proximal reference diameter. A 3.5 x 23 mm scaffold was then implanted with low-pressure inflation in order to avoid vessel injury due to the tapering of the vessel distally.
Immediately after implantation, a proximal postdilation was performed with a 3.75 x 15 mm noncompliant balloon (see Fig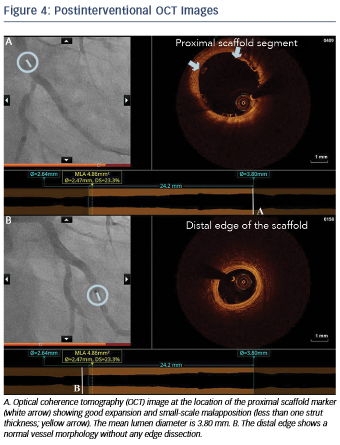 ure 3). A final OCT was performed to assess the implantation result, showing a good scaffold expansion with small-scale malapposition (less than one strut thickness) proximally that was accepted, and absence of vessel injury at the edges of the stent (see Figure 4).
ure 3). A final OCT was performed to assess the implantation result, showing a good scaffold expansion with small-scale malapposition (less than one strut thickness) proximally that was accepted, and absence of vessel injury at the edges of the stent (see Figure 4).
Overall, in this case, OCT helped us to achieve optimal lesion coverage, select the size and length of the implanted scaffold that was different from what was suggested by online QCA and guide the use of proximal postdilation. Moreover, OCT helped confirm the absence of distal vessel injury and a good expansion and apposition.
The publication of this information was supported by St. Jude Medical.