Case study 2. Identification of Mechanism of Stent Thrombosis and Guidance of Treatment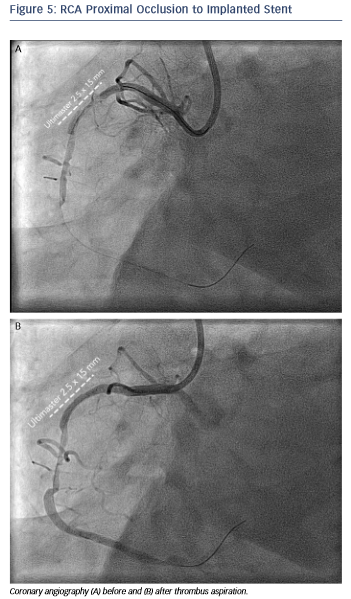
A 68-year-old female had a history of primary percutaneous intervention of the Right Coronary Artery (RCA) two weeks earlier in another hospital with implantation of an UltimasterTM (Terumo Europe, Leuven, Belgium) 2.5 x 18 mm stent due to an acute inferior infarction. She presented in our centre with recurrent inferior ST-elevation myocardial infarction.
The angiogram revealed an occlusion of the RCA proximally to the previously implanted stent (see Figure 5). After thrombus aspiration, a co-registered OCT was performed to investigate the pathomechanism of the stent failure. Cross-sectional OCT images (see Figure 6) revealed the presence of an underexpanded and malapposed stent with thrombotic material at the site of the most severe underexpansion.
Moreover, OCT showed the presence of extensive disease distally to the stent comprising several stenotic lesions (see Figure 7).
Importantly, these findings of excessive malapposition, underexpansion and in-stent stenosis due to thrombus were not visible by angiography, while the severity of the downstream disease was also underestimated. A landing zone was selected based on the lumen profile view, aiming to cover the entire diseased segment. OCT measurements dictated the selection of a P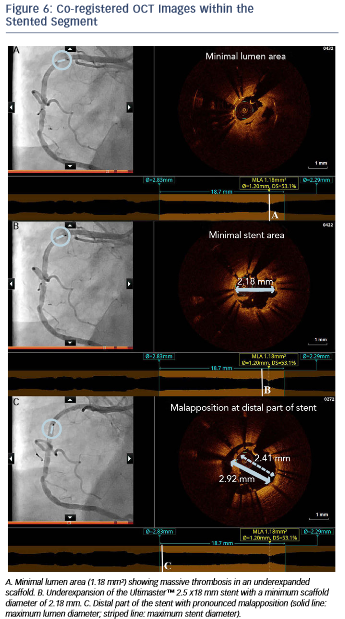 romusTM 3.0 x 32 mm (Boston Scientific, Natick, MA, US), with the intention to distally overlap the pre-existing stent. Immediately postimplantation, after considering the lumen area at the site of the malapposition (2.67 mm) and a distal reference area of 2.82 mm, the balloon of the stent (3.0 mm diameter) was used for postdilation of the entire stented region,
romusTM 3.0 x 32 mm (Boston Scientific, Natick, MA, US), with the intention to distally overlap the pre-existing stent. Immediately postimplantation, after considering the lumen area at the site of the malapposition (2.67 mm) and a distal reference area of 2.82 mm, the balloon of the stent (3.0 mm diameter) was used for postdilation of the entire stented region, 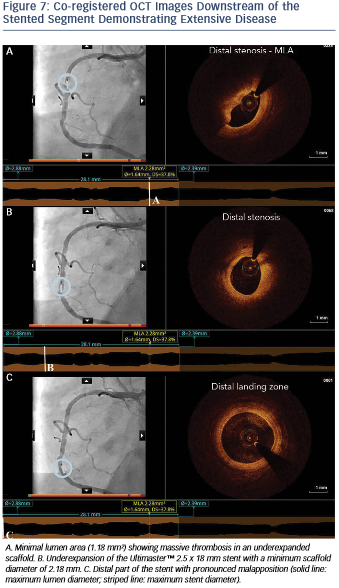 including the underexpanded and malapposed Ultimaster stent. This resulted in a well-expanded stent, landing in a relatively healthy segment and with a short segment of strut overlap (see Figure 8). The lumen area within the previous stent was also improved (Minimal Lumen Area (MLA) increased from 1.18 mm² to 5.29 mm²), as were apposition and expansion of this stent.
including the underexpanded and malapposed Ultimaster stent. This resulted in a well-expanded stent, landing in a relatively healthy segment and with a short segment of strut overlap (see Figure 8). The lumen area within the previous stent was also improved (Minimal Lumen Area (MLA) increased from 1.18 mm² to 5.29 mm²), as were apposition and expansion of this stent.
In this case, OCT helped us understand the pathomechanism of stent thrombosis and also revealed the presence of severe under-recognised atherosclerotic disease distally to the stent. The visualisation of the substrate together with the accurate measurements helped us selected the proper treatment, resulting in optimal lesion coverage and correction of the mechanical issues of the thrombosed stent.
The publication of this information was supported by St. Jude Medical.