A substudy of DISCOVER-FLOW demonstrated considerable accuracy of FFRCT for diagnosis of lesion-specific ischaemia of coronary lesions of intermediate stenosis severity (40 % to 69 %).39 A larger, prospective multicentre clinical trial, the Determination of fractional flow Reserve by anatomic computed tomographic angiography (DeFACTO) study is similarly designed to determine the diagnostic performance of FFRCT for the noninvasive assessment of lesion-specific ischaemia using invasively measured FFR as the reference standard.27 This multicentre diagnostic performance study involving 252 stable patients with suspected or known CAD observed that FFRCT demonstrated improved diagnostic accuracy versus CT alone for diagnosis of ischaemia, although the study did not satisfy its prespecified primary end point of diagnostic accuracy of greater than 70 % of the lower bound of the one-sided 95 % confidence interval. Refinements in FFR computation technology become recently available which included updated proprietary software with quantitative image quality analysis, improved image segmentation, refined physiological models, increased automation, as well as emphasis on the coronary CTA image acquisition protocol to reflect current guidelines.28
By adopting this refined methodology a recent prospective multicentre trial on 254 patients showed that FFRCT exhibits a very high diagnostic performance compared with invasively measured and high specificity of FFRCT, which was markedly better than in a previous evaluati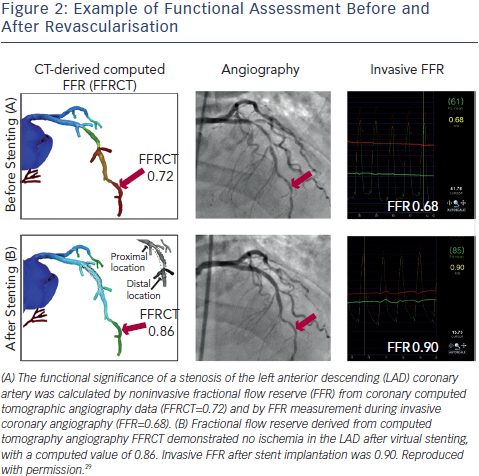 on of FFRCT.21 Moreover, compared with coronary CTA, FFRCT led to a marked reduction in false-positive results. A novel study expedited the application of FFRCT to virtual stenting for the prediction of the functional outcome of stenting prior to the invasive procedure.29 Virtual stenting is performed by modification of the computational model to restore the area of the target lesion according to the proximal and distal reference areas. FFRCT is computed before and after virtual stenting thus providing not only diagnosis of lesion-specific ischaemia but additionally predicts the therapeutic benefit of coronary revascularisation (see Figure 2). FFRCT had a diagnostic accuracy of 96 % in predicting or ruling out myocardial ischaemia after stenting as defined by a post-stent FFR of >0.80 while the mean difference between FFR after stenting and FFRCT after virtual stenting was 0.02 ± 0.05.29 Thus, it appears that comprehensive planning of a revascularisation strategy and selection of the optimal target coronary lesion(s) for revascularisation is possible using this novel technology, which can provide both anatomical and functional information for each lesion before the invasive procedure.
on of FFRCT.21 Moreover, compared with coronary CTA, FFRCT led to a marked reduction in false-positive results. A novel study expedited the application of FFRCT to virtual stenting for the prediction of the functional outcome of stenting prior to the invasive procedure.29 Virtual stenting is performed by modification of the computational model to restore the area of the target lesion according to the proximal and distal reference areas. FFRCT is computed before and after virtual stenting thus providing not only diagnosis of lesion-specific ischaemia but additionally predicts the therapeutic benefit of coronary revascularisation (see Figure 2). FFRCT had a diagnostic accuracy of 96 % in predicting or ruling out myocardial ischaemia after stenting as defined by a post-stent FFR of >0.80 while the mean difference between FFR after stenting and FFRCT after virtual stenting was 0.02 ± 0.05.29 Thus, it appears that comprehensive planning of a revascularisation strategy and selection of the optimal target coronary lesion(s) for revascularisation is possible using this novel technology, which can provide both anatomical and functional information for each lesion before the invasive procedure.
FFRCT is a promising noninvasive method for identification of individuals with ischaemia and the prediction of the functional outcome of revascularisation. These findings can be considered proof of concept of the feasibility of this novel technology and represent the first large-scale prospective demonstration of the use of computational models to calculate rest and hyperaemic coronary pressure fields from typically acquired CCTA images. The calculation of FFR from CT images requires uploading the CT scan digital imaging and communications in medicine (DICOM) image dataset to particular workstations for image analysis, geometric modelling and supercomputer computation. At present, this data is only provided as a service by a single company, which performs the image analysis, geometric modelling and supercomputer computation20,21,26,28,29,39,40 and thus results are not generated at the clinical site. Moreover, this process currently takes several hours per exam, however iterative improvements in automation are expected reduce processing time in the near future.26
A recent investigation sought to project the potential clinical and economic consequences of using FFRCT to guide clinical management, in comparison with commonly used alternative strategies for the diagnosis and treatment of patients with known or suspected CAD and reported that use of FFRCT to select patients for invasive coronary angiography and revascularisation would result in 30 % lower costs and 12 % fewer events at one year compared with the most commonly used strategies.41 Derivation of FFRCT is hampered by certain limitations at the extraction of the vascular structures from CT images, formulation of boundary flow conditions and definition of modelling equations of flow.38 Erroneous segmentations are usually encountered in clinical practice, due to the presence of high attenuation objects such as calcified plaques or stents which produce image artefacts. Following image segmentation the entire volume occupied by the coronary artery is discretised into a large number of small elements, a process known as meshing, which allows for the solution of the blood flow problem at the location of each element. This meshing process is usually user-dependent and potentially introduces further uncertainty in blood flow modelling.
Finally, realistic inflow and outflow boundary flow conditions are required to perform the CFD simulation, however blood pressure cannot be directly measured by CCTA and brachial blood pressure is often used as a surrogate for pressure in large arteries. The outlet boundary condition (which models the effect of the distal vascular system, such as small arteries, microcirculatory vessels and veins and returning blood to the heart) is difficult to determine in practice. Outlet boundaries are derived by coupling the lumped parameters, which approximate the haemodynamic conditions of the distal vascular system.42 The estimated flow distribution of each of the major coronary arteries is a consequence of the relationship between vessel size and resistance, while cardiac output is based on the measurement of myocardial mass that is derived from the cardiac CT dataset. Furthermore, the coronary venous resistance is calculated based on the assumption of mean coronary blood flow at the expense of incorporating patient-specific factors.