Optimum Antiplatelet Therapy in ST Elevation Myocardial Infarction (STEMI)
Patients with STEMI and planned primary PCI require particularly urgent platelet inhibition and represent a group potentially benefiting most from the new antiplatelet therapies.
In the STEMI cohort of the TRITON-TIMI 38 trial prasugrel significantly reduced the primary endpoint of cardiovascular death, non-fatal MI, or non-fatal stroke by 32 % after 30 days (6.5 vs 9.5 %, P=0.0017).18 The absolute risk reduction was 3.0 %. In particular, benefits were seen among patients with anterior STEMI. In comparison to clopidogrel prasugrel reduced the primary endpoint in these patients by 43 % – regardless of a concomitant use of glycoprotein IIb/IIIa blockers. The rate of bleeding complications not related to CABG was similar in the prasugrel- and clopidogrel-group (2.4 vs 2.1 %). However, in patients with bypass surgery TIMI major bleedings occurred more often among those with prasugrel therapy (18.8 vs 2.7 %). In general, the rate of bleeding complications in the STEMI cohort was not increased – despite a use of glycoprotein IIb/IIIa blockers in 60 % of the patients.
In the STEMI cohort of the PLATO trial ticagrelor reduced the primary endpoint of cardiovascular death, non-fatal MI, or non-fatal stroke by 13 % (9.4 vs 10.8 %; P=0.07).19 The absolute risk reduction was 1.4 %. Ticagrelor also reduced several secondary end points, such as MI (HR=0.80; P=0.03), mortality (HR=0.82; P=0.05) and stent thrombosis (HR, 0.66; P=0.03). Ticagrelor did not affect major bleeding (HR, 0.98; P=0.76).
In the Rapid activity of platelet inhibitor drugs primary PCI (RAPID) study pharmacodynamic measurements after administration of prasugrel and ticagrelor loading dose were performed.20 In terms of residual platelet reactivity there were no significant differences after two and four hours between the two agents. Surprisingly, four hours were required to achieve sufficient platelet inhibition in the majority of STEMI patients. Futhermore, morphine use was associated with a delayed activity of prasugrel and ticagrelor.
Interestingly, the guidelines of the European Society of Cardiology (ESC) and the American College of Ca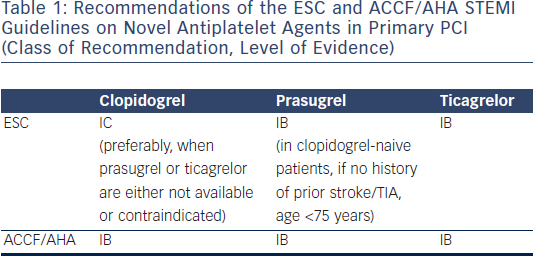 rdiology Foundation/American Heart Association (ACCF/AHA) do not completely agree on the utilisation of novel antiplatelet agents (see Table 1). The STEMI guidelines of the ESC give ticagrelor and prasugrel a IB recommendation.21 However, prasugrel should only be given in clopidogrel-naive patients, if there is no history of prior stroke/TIA and age <75 years. In general, these two novel antiplatelet agents are preferred over clopidogrel. According to the ESC guidelines clopidogrel should only be used (IC recommendation) when prasugrel or ticagrelor are either not available or contraindicated. On contrary, the ACCF/AHA STEMI guidelines do not declare superiority of ticagrelor and prasugrel over clopidogrel.22 All three agents are given a IB recommendation. In the eyes of the American task force an important shortcoming of the prasugrel and ticagrelor data is that there are no specifically designed STEMI trials and only post-hoc secondary analyses exist.
rdiology Foundation/American Heart Association (ACCF/AHA) do not completely agree on the utilisation of novel antiplatelet agents (see Table 1). The STEMI guidelines of the ESC give ticagrelor and prasugrel a IB recommendation.21 However, prasugrel should only be given in clopidogrel-naive patients, if there is no history of prior stroke/TIA and age <75 years. In general, these two novel antiplatelet agents are preferred over clopidogrel. According to the ESC guidelines clopidogrel should only be used (IC recommendation) when prasugrel or ticagrelor are either not available or contraindicated. On contrary, the ACCF/AHA STEMI guidelines do not declare superiority of ticagrelor and prasugrel over clopidogrel.22 All three agents are given a IB recommendation. In the eyes of the American task force an important shortcoming of the prasugrel and ticagrelor data is that there are no specifically designed STEMI trials and only post-hoc secondary analyses exist.
In summary, prasugrel may be best suited for younger STEMI patients with large areas of myocardium at risk (e.g. anterior STEMI) or diabetes who are not planned for CABG and have a low risk of bleeding. Ticagrelor may be the best option for older patients or patients with a moderate bleeding risk and patients with a conservative strategy. Clopidogrel may rather be used in patients with a contraindication for prasugrel and ticagrelor or concomitant chronic anticoagulation therapy.