Case Presentation 1
PCI in a Patient with Dual Antiplatelet Therapy Constraints
Professor Ahmed Khashaba of Ain Shams University in Cairo, Egypt, presented a case of a 45-year-old man with multiple cardiovascular (CV) risk factors; a smoker for 22 years, hypertension for five years and noninsulin-dependent diabetes for two years, with glycated haemoglobin levels (HbA1c) of 7.1 percent. He also had chronic liver disease and bleeding oesophageal varices treated by endoscopic variceal ligation three weeks previously. He presented with a non-ST elevation myocardial infarction (NSTEMI). An electrocardiogram (ECG) showed an infero-lateral ST depression and T-wave changes. Troponin testing was positive, and haemoglobin (Hb) levels were 9.9, indicating anaemia. The patient appeared to have a simple lesion – varifocal stenosis in the right coronary artery (RCA) followed by a mobile small thrombus in the RCA. Several issues needed addressing regarding the treatment of this patient. The interventional strategy was the selection of stent technology; DES, BMS, bio active stent (BAS) or bioresorbable scaffold (BVS); the intra-procedural adjunctive pharmacotherapy and the post-procedural dual antiplatelet therapy (DAPT) strategy. Two interventional cardiologists were invited to discuss how they would treat 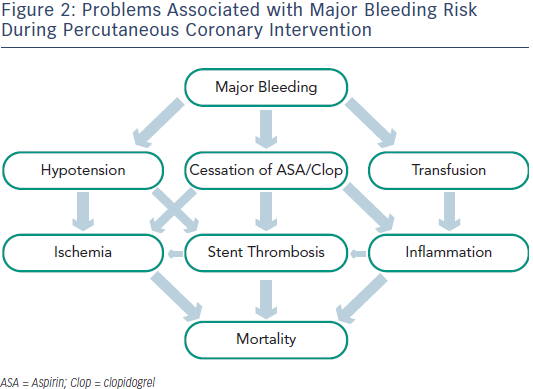 this patient.
this patient.
Professor Giuseppe de Luca of Eastern Piedmont University in Novara, Italy, highlighted the high risk of bleeding complications in this patient. Major bleeding is an important cause of mortality in PCI procedures and is associated with a number of adverse effects, including stent thrombosis (see Figure 2). An observational cohort study found that discontinuation of DAPT was a major determinant of stent thrombosis within the first six months following treatment with DES.7 The highest negative impact of DAPT discontinuation was observed within seven days of discontinuation. For patients with high risk of bleeding complications, several potential strategies are available – balloon angioplasty, drug-eluting balloon (DEB), BMS or a pro-healing stent such as Genous or Avantgarde.
In addition, the reason for DAPT cessation has an impact on cardiovascular risk. Cessation may result from discontinuation resulting from physician recommendation, interruption for surgery followed by resumption of DAPT within 14 days, or disruption due to bleeding or noncompliance. The patterns of nonadherence to anti-platelet regimens in stented patients (PARIS) registry found that the hazard ratio for stent thrombosis was 0.39 following discontinuation (p=0.137); 0.64 following interruption (p=0.664) and 2.58 following disruption (p=0.013). The early risk for stent thrombosis due to disruption was substantial – a hazard ratio of 15.94 at 0–7 days (p=<0.001). The effect was attenuated over time.8
Since this patient is therefore at high risk for stent restenosis, the Cre8 DES represents an attractive compromise between the risk of major bleeding and the risk of stent restenosis. In addition, the patient is young and may have multivessel disease, therefore an aggressive treatment strategy is warranted. Professor De Luca therefore recommended the following – pretreatment with DAPT (aspirin and clopidogrel 300 mg), PCI using a radial approach, fractional flow reserve (FFR) of the left anterior descending artery (LAD) to determine the degree of stenosis, administration of heparin, thrombectomy if required and direct stenting with Cre8, followed by postprocedural protamine and DAPT for three months.
Dr Holger Nef of the University of Giessen, Germany then provided his opinion on how he would treat the patient. Firstly, he made the observation that this is not a case of 1-vessel disease, the RCA is clearly stenosed but there may be intermediate stenosis of the left coronary artery (LCA), which may not have been detected by visual assessment. Dr Nef emphasised the limitations of visual assessment – in a study in which four experienced visual interventional cardiologists compared their visual assessment of lesions to FFR measurements, the experts classified lesions correctly only in approximately 50 % of cases each.9 Dr Nef considered that we have insufficient information about the lesions and need to see more. He therefore recommended FFR in the ramus circumflex (RCX). The FAME II clinical trial indicated that FFR-guided PCI plus the best available medical therapy, as compared with the best available medical therapy alone, is the optimal strategy in stable coronary artery disease (CAD).10
In terms of the choice of stent, the use of a stent that is too short may damage the necrotic core, therefore intravascular imaging is needed. Two other factors should be taken into account; the patient has diabetes, a predictor of in-stent restenosis,11 and also is at a high risk of bleeding. The Zotarolimus-eluting Endeavour sprint stent in Uncertain DES candidates (ZEUS) trial, an open-label randomised clinical trial involving 1,600 individuals, aims to assess whether the use of DES, followed by DAPT, is superior to BMS.12 Outcomes at one year show that major adverse cardiac events (MACE) are lower for patients implanted with a DES compared with a BMS, with less target vessel revascularisation in the DES group and no difference in bleeding events between the two groups.13
Dr Nef recommended the following – clarification of the significance of the lesions in all vessels using FFR, use of intravascular imaging, implantation of a DES and treatment with DAPT (aspirin and ticagrelor) for as long as needed but as short as necessary, not longer than six months.
Professor Khashaba returned to describe how he actually treated this patient. The major difficulty in this case was balancing the risk of bleeding against the risk of thrombosis and restenosis. The bleeding risk was calculated as a HAS-BLED score of four and a Glasgow-Blatchford gastrointestinal bleeding score of 10, indicating a high risk of bleeding. Risk factors for thrombosis/restenosis included the NSTEMI, visible thrombus, diabetes and a long atheroma. However this was in a large vessel (4 mm) with good distal vessel flow. The options were therefore balloon angioplasty, a BMS or a DES. In a patient with such a high bleeding risk, a stent needs to provide the safety of a BMS with the efficacy of a DES. The Cre8 DES (4.00 x 31 mm) was then chosen because of its decreased risk of stent thrombosis.14 The patient was kept only on aspirin because the risk of bleeding from the upper gastrointestinal tract is higher with clopidogrel.
Following stent implantation, the patient did very well, with no recurrence of variceal bleeding and a correction of anaemia. However, 15 weeks later he experienced accelerating angina and anterior dynamic T-wave changes. A lesion in the LAD was detected, and a second Cre8 DES was implanted. FFR would have given this information prior to the initial procedure. A BMS was not considered appropriate because of the evidence of disease progression and the risk of restenosis. The risk of rebleeding was now low and the decision to use clopidogrel passed by a gastroenterologist. The risk of thrombosis was high because of the unstable angina, lack of visible thrombus, diabetes and the fact that the affected vessel was small (3 mm). However, the athermoma was not very long, and a good distal vessel flow was observed. Following stent implantation, short-term DAPT was recommended for three months (clopidogrel 75 mg every other day and aspirin 81 mg/day). This regimen kept the patient’s P2Y12 reaction units (PRU) between 142–155 on serial measurements.
The take-home message from this case presentation was that patients with a high risk of bleeding represent a significant challenge during PCI, even with simple lesions.