Case Presentation 2
PCI in a Patient Undergoing PVI at High Risk of Restenosis
Dr Mathias Vrolix of Ziekenhuis Oost Limburg in Genk, Belgium, presented the case of a 57-year-old female who was obese (body mass index [BMI] 31.7); other risk factors included type 2 diabetes, a familial history of cardiovascular disease (CVD) and hypercholesterolaemia (LDL 3.6 mmol/L). The patient had a recent diagnosis of breast cancer and had undergone a lobectomy six weeks previously. Nodal metastasis had been detected and chemotherapy suggested. Exercise tolerance testing (ETT) was not performed because the patient presented with unstable angina. However, nothing specific was seen on an ECG. The patient was admitted to hospital for diagnostic coronary angiography, which revealed one lesion in the RCA as well as LCA lesions in the circumflex (CX) and LAD. This patient was therefore diagnosed with 3-vessel disease and a SYNTAX score of 14. The FFR in the RCA was 0.77, in the main stem LAD was 0.71 and FFR was not performed in the CX.
Professor de Luca proposed his treatment strategy. He calculated the patient’s SYNTAX score as 26, a score that would have been a clear indication for coronary artery bypass grafting (CABG) several years ago. A recent meta-analysis of 14 clinical trials found that among diabetic patients with multivessel disease and/or left main disease, CABG is superior to DES in terms of mortality.15 However, in this case, the SYNTAX score of 26 is close to the borderline (23). The patient has mostly focal, not complex lesions. The patient is relatively young and has recent cancer with metastases. These factors, together with improved stent technology and DAPT, suggest that a DES may be the appropriate strategy, and the Cre8 stent would be a good choice. The chosen approach was therefore multistep revascularisation, firstly by direct stenting of the RCA and, a few days later, stenting of the left main (LM), LAD and CX. The first step should be administration of DAPT comprising aspirin and prasugrel or ticagrelor. A radial approach should be taken. Professor de Luca recommended the following – administration of heparin and glycoprotein IIb-IIIa inhibitors (bolus) for the LM PCI, implantation of a Cre8 stent, intravascular ultrasound (IVUS) imaging, postprocedural protamine and 12 months of DAPT.
Dr Nef then presented his opinion. This is a case containing three clear stenosis – the RCA is highly stenosed, and stenoses are evident in the LAD and LM. Numerous studies support the use of IVUS to determine the degree of stenosis.16–20 Dr Nef recommended the use of PCI, a decision that is supported by clinical evidence – the FREEDOM trial in patients with diabetes and advanced CAD concluded that coronary artery bypass grafting (CABG) was superior to PCI in terms of rates of myocardial infarction (MI) and death from any cause.21 But that significance between the two techniques was only achieved at five years. At up to two years there was no difference between PCI and CABG.21 In view of the potentially limited life expectancy of a patient with metastatic malignancy, PCI is therefore an attractive choice. In terms of stent choice, a registry study showed that in diabetic patients, DES are associated with half the risk of restenosis compared with BMS, with similar risk of death or MI within four years in both groups.22 The ABSORB Expand trial also demonstrated the benefits of a DES in diabetic subgroups.23 In terms of stenting procedure, a simple without kissing balloon dilatation (FKBD) is recommended as this is associated with reduced use of contrast media and shorter procedure and fluoroscopy times24 Dr Nef therefore recommends a simple procedure involving one stent.
The discussion returned to Dr Vrolix, who outlined how he actually treated this patient. He would have offered CABG since the patient’s life expectancy exceeded two years but the patient refused surgery. The culprit lesion was considered to be the lateral branch of the CX. The first step was peri-procedural management using femoral access and six French, aspirin 80 mg, clopidogrel 600 mg loading dose, heparin 70E/kg according to activated partial thromboplastin time (APTT). Step two was the PCI procedure for the lateral branch. A complication occurred – a fausse route in the lateral branch of the CX resulted in a dissection of the CX. The main stem and LAD were treated as follows – lesion preparation with compliant balloons, stenting of the LAD and then the main stem, 3 x 12 mm and 3.5 x 31 mm.
In step three of the PCI procedure, the main stem was checked and a stent implanted in the posterior descendens RCA (DES, 2 mm, not Cre8). The lateral branch of the CX was rewired, using a Fielder XT guide wire and balloons. Stenting was impossible because of the angle of the lateral branch. A good angiographic result was seen after multiple ballooning. At six months follow-up the patient remained asymptomatic and chemotherapy was uneventful. There were no bleeding complications on DAPT, and DAPT was stopped at six months.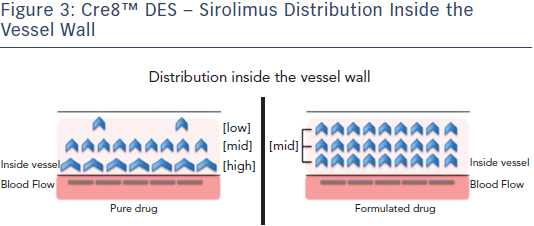
The Cre8 DES was well suited to this complex case. Its structure provides high radial strength, a necessary consideration for use in the main stem. It can be easily positioned and has demonstrated efficacy in diabetic patients.6 It employs a fatty acid, which acts as a permeation enhancer, in its formulation. Fatty acids are used to improve transdermal and skin delivery of drugs,25 and cardiac fatty acid uptake is increased in diabetic mouse models.26 This combination of drug and permeation enhancer leads to increased drug concentration in the tissue, allowing a homogeneous distribution and a uniform action on the whole tissue (see Figure 3).