Clinical Safety
A perception persists that the percutaneous treatment of coronary CTOs is associated with significant procedural and patient risk.4 This however is not reflected in the published data in the modern literature that reflects contemporary practise. In the largest published meta-analysis, examining over 18,000 patients undergoing a CTO PCI procedure from 65 studies in the era 2000–11, there was an overall rate of major adverse cardiovascular events (MACE) of 3.1 % (pooled estimate, 95 % CI:2.4 %–3.7 %).10 Specifically, the overall procedural mortality was 0.2 %, with the commonest 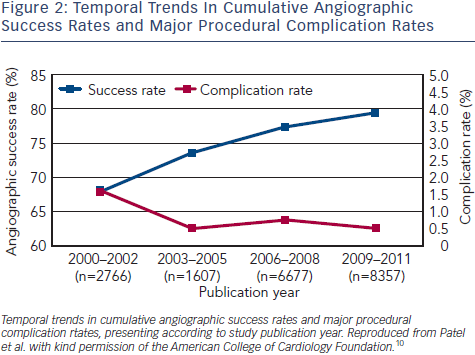 procedural complications being perforation (2.9 %, 95 % CI: 2.2 %–3.6 %) and contrast nephropathy (3.8 %, 95 % CI: 2.4 %–5.3 %). Overall, the success rate across the cohort was 77 %, with evidence that this has improved progressively year on year during the duration of the study (see Figure 2). The authors were able to study the impact of the retrograde approach in over 886 lesions (884 patients), and reported an similar overall MACE rate (3.1 %), driven predominately by periproceduralMI (2.8 %), but with a lower rate of procedural mortality (0.1 %). The success rate of the retrograde approach is comparable to that of the overall cohort at 79.6 %.
procedural complications being perforation (2.9 %, 95 % CI: 2.2 %–3.6 %) and contrast nephropathy (3.8 %, 95 % CI: 2.4 %–5.3 %). Overall, the success rate across the cohort was 77 %, with evidence that this has improved progressively year on year during the duration of the study (see Figure 2). The authors were able to study the impact of the retrograde approach in over 886 lesions (884 patients), and reported an similar overall MACE rate (3.1 %), driven predominately by periproceduralMI (2.8 %), but with a lower rate of procedural mortality (0.1 %). The success rate of the retrograde approach is comparable to that of the overall cohort at 79.6 %.
The incorporation of Bridgepoint™ technology into the hybrid strategy for the treatment of CTOs has led to its adoption in CTO practice despite no large scale published data on the safety of controlled dissection re-entry using the system.11 The largest single-centre series published to date utilised the approach in 62 consecutive cases (60 patients) and have reported follow-up data for a median duration of 1.8 years. When compared to a demographically similar cohort of patients that underwent a CTO procedure over the same time scale that did not utilise Bridgepoint™ technology, overall success rates were similar to that quoted in the wider literature (Bridgepoint™ vs Non-Bridgepoint™: 74.2 % vs 75.4 %; p=0.99) and there were no significant differences in immediate procedural complication rates (Bridgepoint™ vs Non Bridgepoint™: overall complication rate 8.2 % vs 8.3 % (p=0.99); Perforation rate 1.6 % vs 3.2 % (p=0.99); vascular site complication 7.6 % vs 3.6 %: p=0.27). There was a higher (nonsignificant) rate of procedural MI reported in the Bridgepoint™ group (13.2 % vs 7.2 %, p=0.25) but the clinical impact of this remains uncertain. It is important to note, however, that within the Bridgepoint™ group, a significantly higher proportion of patients had already had one unsuccessful attempt (1.6 % vs 13.1 %; P=0.01) at CTO PCI by an alternative strategy. This indicates that controlled dissection-reentry using Bridgepoint technology is a safe and effective technique that offers a reproducible way to facilitate procedural success in CTOs that in many cases would remain untreatable.11 However, long-term multicentre clinical outcome data remains unavailable, as do randomised controlled trials.
When compared to an overall procedural mortality rate of 0.65 % for all PCI undertaken outside of ST segment elevation myocardial infarction (STEMI) (excluding cardiogenic shock)12, CTO PCI using both traditional and hybrid techniques can be considered safe. Of course, such published data is derived from a series of cohort analysis in whom the operators were expert practitioners. Given the learning curve for new CTO PCI techniques, the current recommendations advocate that CTO intervention should be undertaken by those individuals that have a specific interest in CTO intervention and who have undergone specialist training.1 There is evidence that having procedural guidance by visiting highly experienced proctors in the catheter lab significantly improves procedure success rates and shortens the learning curve9 Conceptually, however, CTO PCI (including retrograde techniques) is safe, with a low overall complication rate.
Clinical Benefits
The underlying justification behind an attempt at CTO recanalisation is the relief of myocardial ischaemia in an area supplied by an occluded artery. This may manifest either as symptomatic angina/ angina equivalent, or if asymptomatic, to involve a sufficient extent of myocardium be of sufficient quantity on a non-invasive ischaemia test as to carry prognostic significance. Whilst the relief of symptoms is clear cut, the objective data to support a prognostic benefit for CTO PCI purely on the grounds of the amount of reversible ischaemia is circumstantial and derived from indirect cohort analysis rather than from prospective randomised studies. The following section will describe the data that supports CTO intervention:
Symptomatic Angina
Numerous studies have demonstrated that successful CTO intervention is effective at reducing angina.13,14 Specifically, in patients with clear angina symptoms (CCS 3–4), successful CTO intervention is associated with an early improvement in angina frequency, physical limitation and quality of life (QoL),14 when compared to those patients in which CTO recannulisation was unsuccessful.
However, amongst patients who have minimal symptoms of angina (defined in one study as having an angina frequency score of <100 and termed asymptomatic), only modest non-signifiant improvements in both angina frequency and QoL were noted after successful PCI. Amongst this group, there were no significant differences noted in angina frequency or QoL score if the PCI procedure was successful or not, along with no differences in 30-day mortality (see Figure 2).14 There remains no long-term systematic follow-up data to assess the overall impact on mortality/prognosis in this cohort of asymptomatic patients.
In addition to the improvement in symptoms, successful CTO intervention can lead to demonstrable improvements in left ventricular function,15–17 and a reduction in ventricular arrhythmias18 when completed in patients with impaired left ventricular systolic function. In addition, a number of observational studies have demonstrated a reduction in the need for coronary bypass surgery in those patients who have undergone a successful CTO PCI procedure.1 All these data were derived from patients who presented with symptomatic angina. By contrast, there are, at present, no specific data to support CTO revascularisation with the aim of improving left ventricular function or preventing ventricular arrhythmia’s in patients who do not have manifest angina. There are ongoing trials in this area that are due to report in 2016–17 (see below).