Stent Materials, Design, Longitudinal Strength and Stent Fracture
Metallic stents are manufactured by different processes. These include laser cut slotted tubes, multilink hoops and the sinusoidal continuous wire, which is a single unit that is wound, folded and welded into shape. The stent must apply sufficient radial force on the wall of the diseased coronary artery so that the vessel lumen is restored to a near normal diameter whilst subsequently scaffolding the vessel and preventing collapse of the artery in the longer term. Desirable performance characteristics include low elastic recoil, conformability, high visibility and ease of deliverability. The latter is a complex parameter influenced by the flexibility afforded by the stent itself, the properties of the delivery balloon system and the overall crossing profile of the entire device.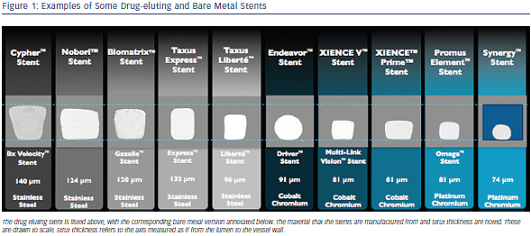
Mechanical engineering is a science of compromise. Therefore, altering any single feature of a stent inevitably affects other properties. There is a complex interaction between every feature of stent design and how the device behaves in clinical practice.13The radio-opacity of a stent is mainly dictated by the material (usually a metallic alloy) from which it is constructed, where the resistance to penetration by X-ray is proportional to the cube of the atomic number of the elements that make up the alloy.13 There are a range of metallic alloys that are employed in commonly used stents. These include stents that are constructed from 316L stainless steel, cobalt chromium alloys (MP35N and L605) and platinum chromium alloys (see Figure 1 and Table 1 for examples). The alloy that the stent is constructed from will not only alter the radio-opacity but also the elastic modulus (a material’s tendency to be deformed elastically or non-permanently when a force is applied to it), yield strength (the stress at which a material exhibits plastic or permanent deformation) and tensile strength (the maximum stress that a material can withstand whilst stretched or pulled before its cross-sectional area significantly contracts).14 In clinical terms, these latter features dictate the overall radial strength of the stent itself, in addition to its susceptibility to recoil. These two features are not mutually exclusive. However, these properties are crucial for both the acute and long-term performance of the stent. The evolution away from stainless steel towards other alloys has been to allow the stent struts to become thinner whilst maintaining the overall radial strength of the device.
Most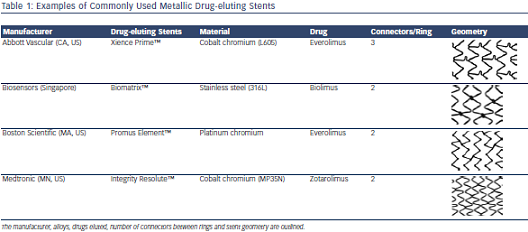 recently, bioresorbable stents have been introduced to the clinical arena. The most extensively studied stent is currently the Absorb™ (Abbott Vascular, Santa Clara, CA, US). This stent is manufactured from a poly-L-lactic acid (PLLA) polymer. This semi-crystalline polymer is constructed from a number of linked sinusoidal hoops with stent struts that are 150 μm thick.15 This particular stent cannot be seen radiographically and has two small metallic markers sited at the distal and proximal stent edges for intra-procedural identification. A number of other bioresorbable materials and platforms are under investigation at various stages,15 although a review of these materials and devices is beyond the scope of this article. Nevertheless, the same mechanical constraints and desirable properties are also directly applicable to these devices.
recently, bioresorbable stents have been introduced to the clinical arena. The most extensively studied stent is currently the Absorb™ (Abbott Vascular, Santa Clara, CA, US). This stent is manufactured from a poly-L-lactic acid (PLLA) polymer. This semi-crystalline polymer is constructed from a number of linked sinusoidal hoops with stent struts that are 150 μm thick.15 This particular stent cannot be seen radiographically and has two small metallic markers sited at the distal and proximal stent edges for intra-procedural identification. A number of other bioresorbable materials and platforms are under investigation at various stages,15 although a review of these materials and devices is beyond the scope of this article. Nevertheless, the same mechanical constraints and desirable properties are also directly applicable to these devices.
A major factor in stent design is the geometry of the stent cell structure (see Table 1). This is dictated by the number and pattern of connectors between rings or hoops. Reducing the number of fixed connectors is potentially desirable as this improves flexibility, delivery and decreases the metal:artery ratio. However, this also potentially impacts negatively on longitudinal strength. It has recently become apparent that longer, thinner and more flexible stents can be less stable in their longitudinal axis. These stents can be ‘compressed’ or distorted along the length of the device creating a ‘concertina’ effect or longitudinal stent deformation (LSD).16,17 This phenomenon is now well-understood and usually relates to an interaction between guiding catheters and stents deployed in the aorto-ostial position, or stents that are relatively undersized after initial deployment that are subsequently ‘caught’ and distorted by secondary equipment that is passed into the coronary vessel.14,16
With regard to longitudinal stability, there are several technical design factors that are associated with an increased susceptibility to LSD. It has been shown that at compressive forces of 50 gF (0.5 N) or less, it is possible to shorten18 or elongate19 modern metallic stents. Stent alloy and strut thickness appear to be somewhat less important with regard to susceptibility to LSD. The construction of the device, number of connectors between rings and their geometrical distribution across the device dictate the longitudinal strength of the platform. In general, more connectors between rings correlate with increasing longitudinal strength. Where connectors are present, those that are in longitudinal alignment confer increasing strength, whilst offset connectors are less strong. However, there is a significant downside to increasing the longitudinal strength of the device. This will increase the ‘stiffness’ of the stent, therefore reducing its deliverability to and conformability within the vessel.
Whilst unrecognised, LSD has the potential to be clinically disastrous for the patient. However, these events appear to be relatively rare.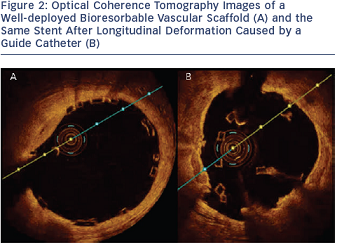
Where LSD does occur, a three-pronged approach is required to manage the stent deformation. Ideally, preventative measures should be undertaken, such as prudent guide catheter selection in ostial lesions to allow for sufficient support without excessive guide engagement. Choosing a stent of an appropriate size and careful proximal stent optimisation (usually with softer semi-compliant balloons in our practice), particularly in the left main stem, will help to ensure that secondary devices are unlikely to catch on struts and cause deformation. Secondly, a low threshold is required for suspecting stent deformation, particularly when there is resistance in delivering post-dilation balloons. Careful fluoroscopy examination and or additional imaging with intravascular ultrasound (IVUS)/optical coherence tomography (OCT) may be necessary to diagnose this problem.16 Finally, if longitudinal stent compression has occurred, cautious post-dilation should be attempted. Small diameter balloons may initially be required to cross the damaged stent, and these can be gradually upsized as necessary. This method has been used with success in our experience.16 Further proximal stent deployment may be needed in the setting of vessel damage.14,16 It is worth noting that this phenomenon can also occur with bioresorbable platforms (see Figure 2). Should this occur, OCT will be necessary to demonstrate the complication.
Nevertheless, there is a clear trade-off with increasing the stiffness of a stent. Whilst longitudinal stability rises with the number of stent connectors, the risk of stent fracture increases as the stent becomes stiffer. Therefore, older stent platforms are much more susceptible to this phenomenon. In one clinical study, the 6-connector Cypher stent was more than four-times more likely to fracture than newer platforms.20 The incidence of stent fracture with the Nobori™ 2-connector Biolimus eluting stent (Terumo Corporation, Tokyo, Japan) is reported at >4 % per lesion at nine-month angiographic assessment in a study of >1,000 patients.21 This may relate to the exact shape of the connector between rings for this particular stent. Fracture has also been described in the thinner strut, 3-connector Xience™ stents (Abbott Vascular, Santa Clara, CA, US) where a combination of LSD and stent fracture were also associated with adverse clinical events.22 This was particularly likely to occur at areas of stent overlap. Another study has suggested an incidence of stent fracture in Xience stents at almost 3 % in a large cohort of >1,000 patients undergoing follow-up angiography between 6 and 9 months.23 Stent fracture is likely to lead to ISR, acute or chronic occlusion and is certainly not a benign phenomenon.20–23 These events are predisposed by certain features within the lesion or vessel. These include treating the right coronary artery, using longer stents, areas of tortuosity, calcification, stent malapposition and stenting at hinge points.
Therefore, whilst LSD can occur as a sudden and dramatic event that complicates a PCI, this can usually be managed and resolved provided that it is recognised. Our experience is that patients do well over the long term when this is the case. In contrast, stent fracture is much more difficult to predict and it also seems to be a more common phenomenon than was previously considered to be the case. Furthermore, there is a high chance of an adverse outcome with stent fracture. Whilst LSD is certainly not desirable, the trade-off of a more flexible and conformable stent platform with less axial stability may be worthwhile if these platforms prevent later complications that are likely to occur in significant numbers. This is becoming increasingly relevant in the era of treating long segments of disease with stents that can be as long as 48 mm and the frequent need for overlapping stents (as is common when treating chronic total occlusions). Newer approaches have been adopted more recently. For example, the Promus Premier™ and Synergy™ II stent models (Boston Scientific, Natick, MA, US) aim to retain flexibility through the body of the stent by using two offset connectors. However, the most proximal three rings are linked by extra connectors to provide resistance to LSD.