Stent Models Across a Product Range, Bifurcations and Over-expansion
It is imperative that cardiologists are intimately familiar with the stents that they use. A differing range of stents occur within the various manufacturer product ranges (see Table 2). Understanding the differences between the stents within these product ranges is key to obtaining a good clinical outcome for the patient. This is becoming more important as the lesion complexity increases. For example, using a two-stent strategy at a bifurcation could potentially have a vastly different mechanical result depending on which product is chosen. If a 2.5 mm diameter product is brought from a side branch back into a much larger diameter main vessel, the final expansion in the proximal main vessel and stent cell diameter (and thus lumen achieved in the main vessel) will be very different than if a 3 mm or 4 mm version of the ‘same stent’ is deployed in the side branch instead. Understanding the implications of these choices is crucial. This is particularly pertinent when the left main stem (LMS) is being treated.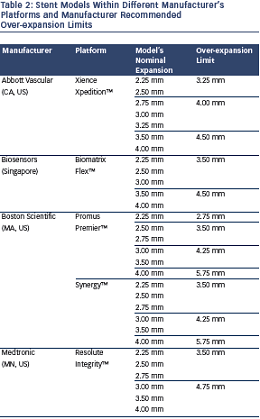
With LMS intervention, over-expansion of current stent platforms is frequently required as the devices are brought back from smaller diameter daughter vessels (LAD or left circumflex). Despite bench testing demonstrating that current drug-eluting stent platforms can maintain structural integrity beyond the nominal expansion diameter,24 there are theoretical concerns that over-expansion may affect drug delivery and cause mechanical disruption of the stent.
The first concern regarding over-expansion is that it may damage the stent polymer, leading to uneven drug elution, with a potential for later ISR.25 Bench testing of over-expansion of first generation DES found that balloon dilation induced only minor polymer coating abnormalities, which have also been noted on undeployed DES.26,27 It is also possible to replicate this polymer damage by delivering stents through tortuous and calcified vessels. Another concern with respect to over-expansion is the risk of mechanical disruption of the stent. Stent fracture is possible with overly aggressive stent expansion.
A further mechanical issue with over-expansion that has been queried is of the potential for stent recoil. This is a theoretical concern due to a reduction in metal:artery ratio and an alteration of the scaffold itself. Stent recoil has been described when treating atheromatous vessels.28 However, in the LMS the usual reason for over-expansion is apposition to the non- diseased vessel wall rather than scaffolding flow limiting plaque. Furthermore, the radial strength of the stent paradoxically increases as it is over-expanded. This is due to straightening of both the ring and connectors, thus leading to greater strength, not less.
Our experience of LMS PCI is that this is typically a very large vessel. In a study of 125 patients, the mean cross-sectional area of the distal LMS was 22.6 mm2 (standard deviation [SD] ± 5.4 mm2) and mean maximal vessel diameter was 5.7 mm (SD ± 0.7 mm).29 Therefore, the vast majority of patients would consequently require post-dilation beyond the nominal diameter of all of the large vessel platforms of current generation DES during LMS PCI. We also performed a further prospective clinical study where all patients who underwent IVUS-guided LMS PCI and stent post-dilation beyond suggested expansion limits were entered into a registry. In 31 patients, mean maximal stent diameters of >5.0 mm were reliably achieved (using Biomatrix Flex™ 9 crown and Promus Element Large vessel platforms) with 5.5 mm and 6.0 mm post-dilation balloons. No intra-procedural complications occurred and in 13.4 months of follow-up only one patient experienced clinical ISR.29 This indicates excellent short-term efficacy and no increased complication rate with over-expansion of current generation DES in the LMS. These results compliment the bench data of Foin et al., but in the clinical arena.24 It should be noted that under-expansion or incomplete stent apposition of BMS or DES is strongly associated with ISR and stent thrombosis.30–32 We would suggest that leaving undersized and unapposed or malapposed stents in the LMS should be avoided at all costs.