Treatment of Central Sleep Apnoea
Although available information is limited, home oxygen therapy has been shown to have some beneficial effects in patients with CSA and HF, with significant reductions in AHI of about 50 %.73,74 Data from two studies in Japanese patients with New York Heart Association (NYHA) class II or III HF-rEF and CSA/CSR were reported in three 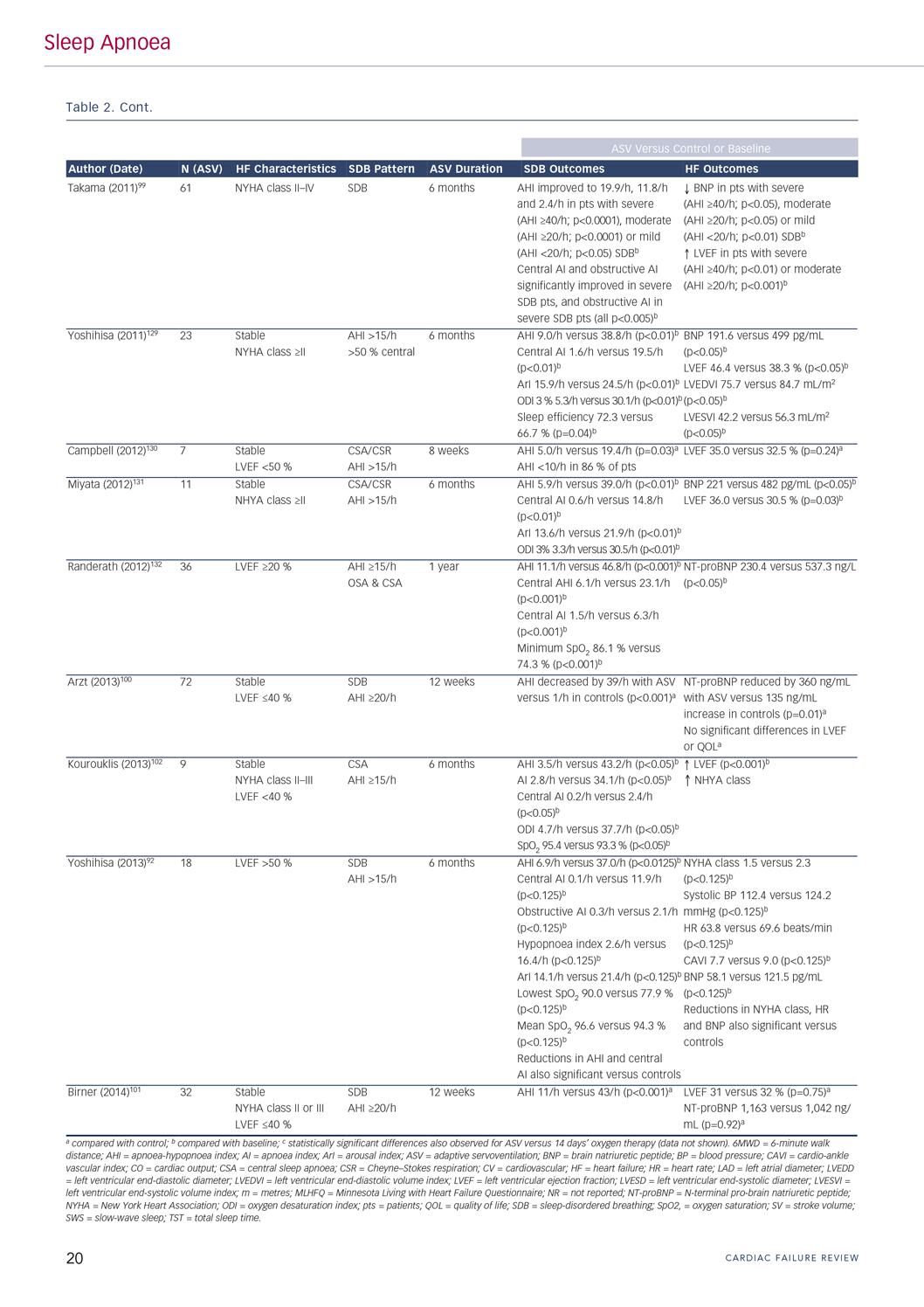 separate publications.75–77 After 12 weeks home oxygen therapy, significant decreases were seen in the AHI (from 21/h at baseline to 10/h; p<0.001), the ODI (from 19.5/h to 5.9/h; p<0.001) and the Specific Anxiety scale score (from 4.0 to 5.0; p<0.001), and LVEF was significantly increased (from 34.7 % to 38.2 %; p=0.022).75 In a separate study, continuing treatment for one year showed that home oxygen therapy was well-tolerated and that the benefits of treatment were maintained over the longer term.76 A post hoc analysis of data from both trials showed that home oxygen therapy had no effect on the number of premature ventricular contractions, although there was evidence of benefit in the subgroup of patients with NYHA class >III and an AHI of >20/h.77 A study conducted in France in a similar patient population also showed that nocturnal oxygen therapy significantly decreased the central AHI and ODI compared with baseline, with treatment effects evident within 12 hours of initiating therapy and persisting during the six-month treatment period.78 In this study, oxygen therapy had no significant effects on the obstructive or mixed AHI values, quality of life or ventricular function.
separate publications.75–77 After 12 weeks home oxygen therapy, significant decreases were seen in the AHI (from 21/h at baseline to 10/h; p<0.001), the ODI (from 19.5/h to 5.9/h; p<0.001) and the Specific Anxiety scale score (from 4.0 to 5.0; p<0.001), and LVEF was significantly increased (from 34.7 % to 38.2 %; p=0.022).75 In a separate study, continuing treatment for one year showed that home oxygen therapy was well-tolerated and that the benefits of treatment were maintained over the longer term.76 A post hoc analysis of data from both trials showed that home oxygen therapy had no effect on the number of premature ventricular contractions, although there was evidence of benefit in the subgroup of patients with NYHA class >III and an AHI of >20/h.77 A study conducted in France in a similar patient population also showed that nocturnal oxygen therapy significantly decreased the central AHI and ODI compared with baseline, with treatment effects evident within 12 hours of initiating therapy and persisting during the six-month treatment period.78 In this study, oxygen therapy had no significant effects on the obstructive or mixed AHI values, quality of life or ventricular function.
The rationale for testing CPAP in patients with CSA and HF was that improving cardiac function by applying PAP would attenuate central SDB. Positive effects associated with CPAP therapy in patients with HF (usually HF-rEF) and CSR include improved LVEF and reduced AHI,68,79–81 but other studies have failed to document statistically significant improvement in outcomes when using CPAP to treat HF patients with CSA/CSR.82–84 Given significant heterogeneity between studies in approaches to CPAP titration, it is possible that therapy failure may be due to inadequate titration and inadequate reductions in AHI during treatment. A good example of this is the Canadian Positive Airway Pressure Trial for Heart Failure Patients with Central Sleep Apnea (CANPAP) study, a randomised controlled trial that investigated mortality in patients with HF-rEF and CSA/CSR treated with CPAP. The study was stopped prematurely after enrolment of 258 of the planned 408 when analysis did not show a beneficial effect of CPAP treatment on survival.85 However, a post hoc evaluation suggested that morbidity and mortality might be improved if there was an early and significant reduction in AHI to <15/h during CPAP therapy.86 Other data suggest that even if CPAP therapy is appropriately titrated there may be a subgroup of patients who do not respond to this treatment option.87,88 Meta-analysis showed a residual mean AHI of 15/h across eight included studies despite CPAP treatment.79 This lack of efficacy may limit the utility of CPAP in some HF patients, while others may have issues with tolerability.89 Recommendations vary, with some suggesting that the wide availability of, 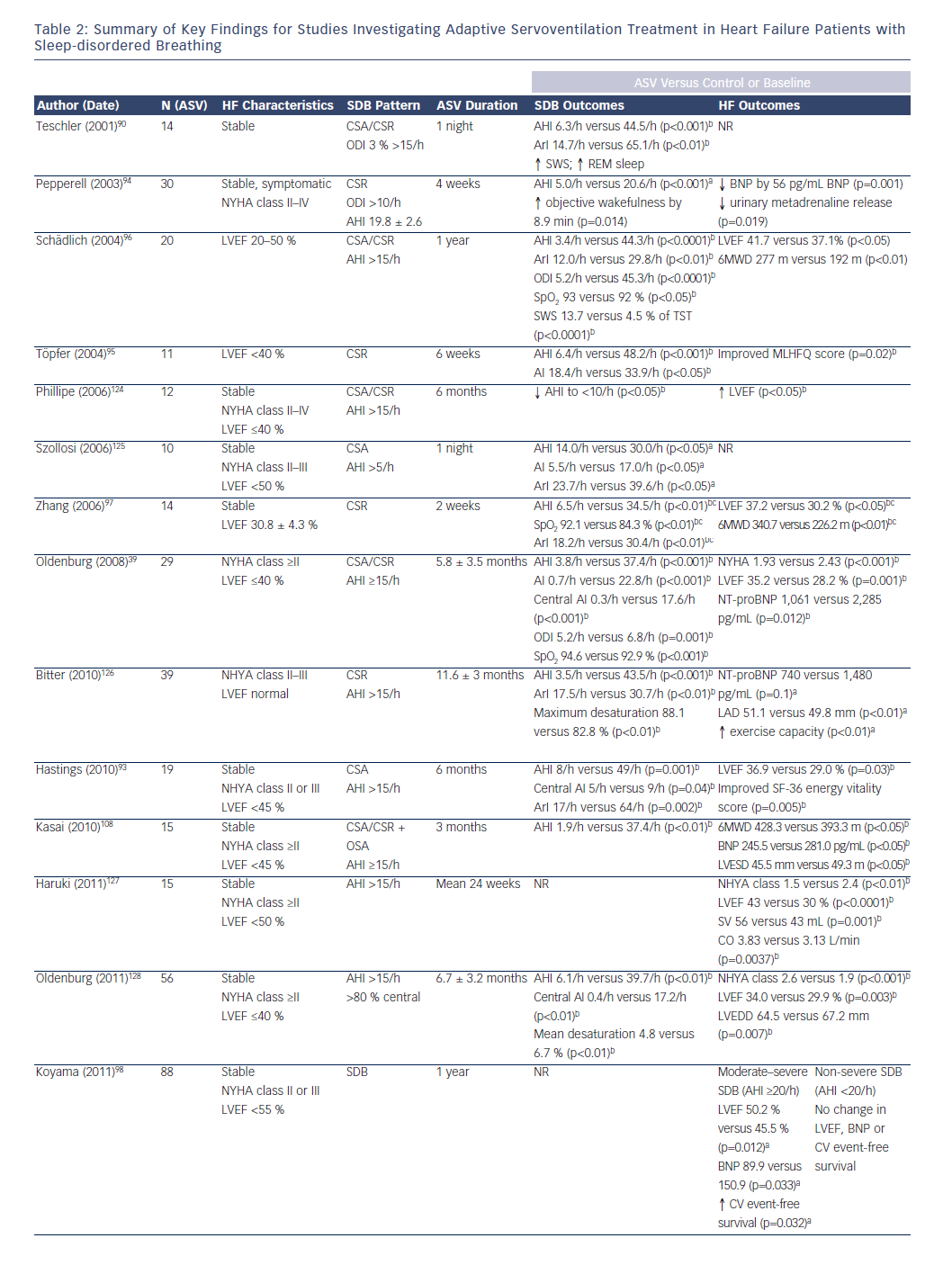 and familiarity with, CPAP means that this approach should be considered for initial treatment of CSA related to HF,79 while others say that CPAP should not be considered as standard therapy for this indication.9 Even if a CPAP trial is undertaken, an alternative treatment option needs to be considered when there is inadequate apnoea suppression.79
and familiarity with, CPAP means that this approach should be considered for initial treatment of CSA related to HF,79 while others say that CPAP should not be considered as standard therapy for this indication.9 Even if a CPAP trial is undertaken, an alternative treatment option needs to be considered when there is inadequate apnoea suppression.79
One such alternative for CSA/CSR in HF is ASV. A varying amount of inspiratory pressure (inspiratory positive airway pressure, IPAP) supports inspiration with decreasing breathing amplitude, and can also ensure sufficient inspiration when breathing efforts are absent.90,91 Different technologies use different methods to stabilise the breathing pattern, with monitoring of minute ventilation being the most widely used. ASV also ensures upper airway patency by providing a fixed or variable amount of end-expiratory positive airway pressure (EPAP), so concomitant OSA will also be treated. Given the different ASV devices and algorithms on the market, it is not clear whether effects of one device can be extrapolated to another.
There is currently no consensus on whether treatment for CSA in HF should be initiated and what the optimal strategy might be. A number of smaller studies have documented improvements in symptoms, cardiac function, cardiac disease markers, exercise tolerance, short-term prognosis and quality of life when ASV treatment has been used in patients with HF and SDB, including CSR (see Table 2).39,92–102 The majority of studies have been conducted in patients with HF-rEF, but beneficial effects of ASV on respiratory and cardiovascular parameters have also been documented in patients with HF-pEF.92 Data from a recent meta-analysis showed that ASV significantly improved AHI, left ventricular function and exercise capacity compared with control in patients who had CSA and predominantly HF-rEF.103 Beneficial changes in sympathetic nervous system activity assessed by microneurography have also been documented.104 There were significant correlations between changes in the AHI and changes in both sympathetic nervous system activity and LVEF.104
Data from comparative studies provide some indication that ASV is a successful method for treating CSA/CSR in HF,90,105–107 although evidence from randomised controlled parallel-group trials is currently lacking. ASV appears to be more effective than CPAP, BPAP and oxygen therapy for treating CSA/CSR in HF,90,105,106 and it has been reported that patients prefer ASV over both CPAP and BPAP.90 In one randomised, open-label study of HF-rEF patients, compliance with therapy (an important aspect of the effectiveness of treatment) was significantly better with ASV compared with CPAP (5.2 versus 4.4 h/night, respectively, p<0.05).108
The influence of effectively treating CSA/CSR in patients with HF-rEF on objective ‘hard’ outcomes such as mortality in randomised clinical trials remains to be determined. Data from the ongoing Treatment of Predominant Central Sleep Apnoea by Adaptive Servo Ventilation in Patients With Heart Failure (SERVE-HF) (NCT00733343),109 Effect of Adaptive Servo Ventilation on Survival and Hospital Admissions in Heart Failure (ADVENT-HF) (NCT01128816)110 and Cardiovascular Improvements With MV ASV Therapy in Heart Failure (CAT-HF) (NCT01953874)111 trials (see Table 3) will help to answer these important questions.
A new treatment option for CSA currently under investigation is phrenic nerve stimulation. Preliminary data show that phrenic nerve stimulation with an implantable pacemaker can treat central apnoeas and thus attenuates respiratory abnormalities and reduces AHI by 50 %, but cannot treat hypopnoeas or other respiratory events.112 Trials to evaluate the clinical effect of this method on HF outcomes are not yet available.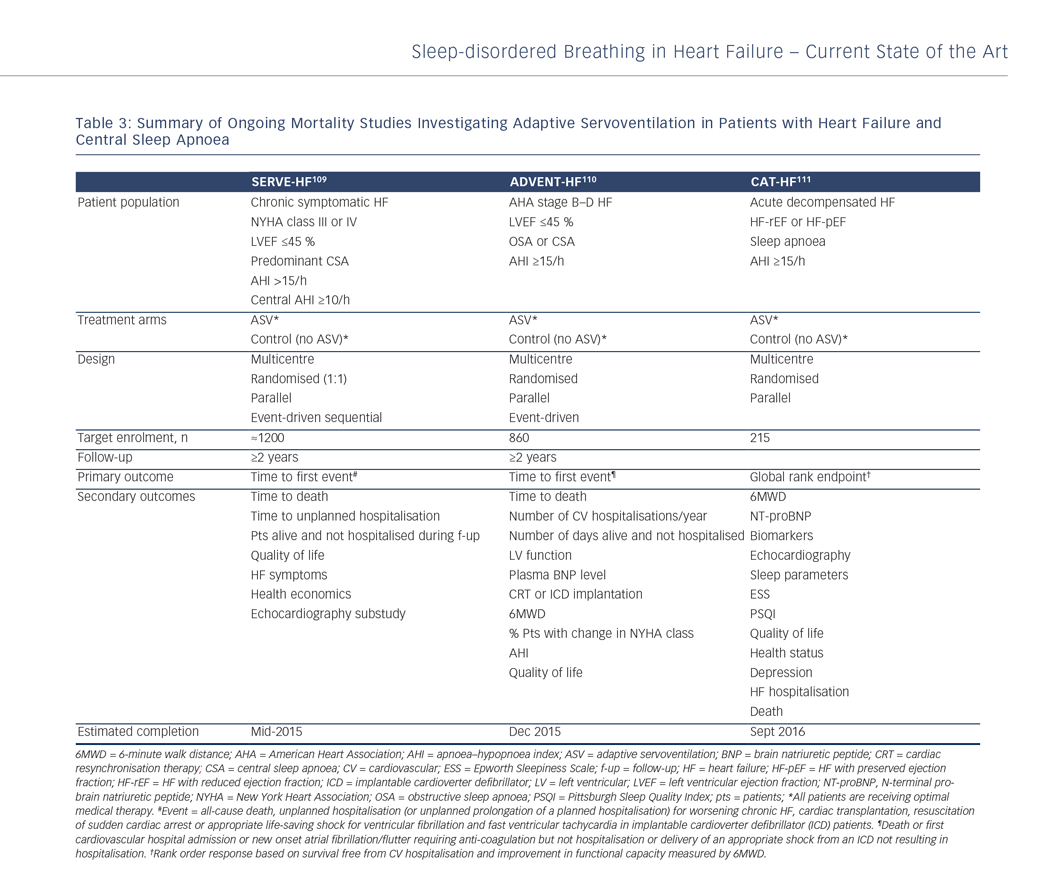
Compliance with Positive Airway Pressure Therapy
Compliance in the context of PAP therapy refers to the consistency with which a patient uses the prescribed treatment. A number of studies have investigated the level of compliance required by OSA patients for the beneficial effects of CPAP therapy to be achieved, be that improved survival,113 decreases in BP,114–117 or improvements in sleepiness118–121 or memory.122 For example, one study analysing the dose–response relationship between CPAP therapy and cardiovascular mortality found evidence that increased usage correlates with improved survival rates, with a significant difference in five-year survival between patients using CPAP for <1 h/day compared with those using CPAP for 1–6 or >6 h/day.113 Similarly, a per-protocol analysis of randomised clinical trial data suggested that CPAP might reduce the incidence of hypertension or cardiovascular events in patients who were adherent to therapy for ≥4 h/night.123 While these studies were not specifically conducted in HF patients, they suggest that a minimum duration of PAP therapy usage will be required for the beneficial effects of treatment to be realised in HF patients. In addition, the relative lack of SDB symptoms in patients with HF might make compliance with therapy more difficult to achieve, meaning that strategies to improve compliance are more important.