Cardiovascular Magnetic Resonance Applications of Special Interest for Cardiovascular Evaluation in Systemic Diseases
Measurement of Volumes – Ejection Fraction
CMR measures ventricular volumes and ejection fraction non-invasively and without contrast agent.6 Due to its high reproducibility, it is ideal for serial follow-up of ventricular volumes, mass and function; compared with echocardiography, which is an operator-dependent technique, with the limitations of acoustic window, CMR is operator-independent and has high reproducibility.7
The majority of CMR data regarding volumes and mass in systemic disease are referred to patients with metabolic diseases and mainly to diabetes mellitus. In patients with type 1 diabetes mellitus (T1DM), it was documented by CMR that in addition to traditional cardiovascular disease risk factors, elevated mean haemoglobin A (1c) and macroalbuminuria were significantly associated with alterations in left ventricular (LV) structure and function.8 In overweight and obese women, insulin resistance is associated with increased cardiac remodelling and reduced diastolic function, assessed by CMR.9 Finally, osteoprotegerin (OPG) was inversely associated with aortic distensibility, LV volumes and LV diastolic function assessed by CMR, while adipocytokine adiponectin (ADPN) was positively associated with myocardial glucose metabolism (MMRglu) by 18F-2-fluoro-2-deoxy-D-glucose positron emission tomography.10 In another study, CMR was used to assess the effect of rosiglitazone on cardiovascular performance and cardiac function in type 2 diabetes mellitus (T2DM) and proved that rosiglitazone increased peripheral oedema but had no pernicious effects on cardiovascular performance or cardiac function, with modest improvement in selected CMR measures.11 Although insulin and glucose indices are associated with abnormalities in cardiac stru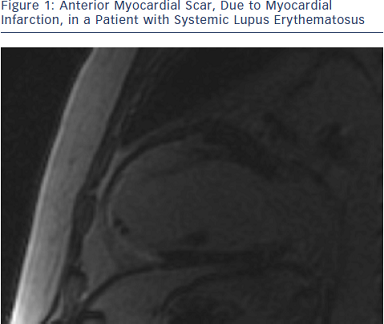 cture, insulin resistance and worsening glycaemia are consistently and independently associated with left ventricular mass (LVM)/LV end-diastolic volume (LVEDV). These data implicate hyperglycaemia and insulin resistance in concentric LV remodelling.12
cture, insulin resistance and worsening glycaemia are consistently and independently associated with left ventricular mass (LVM)/LV end-diastolic volume (LVEDV). These data implicate hyperglycaemia and insulin resistance in concentric LV remodelling.12
CMR also documented that few patients with HIV may have a marginally reduced right ventricular ejection fraction (RVEF) but normal right ventricular (RV) dimensions and mass.13
Finally, the progression to heart failure in rheumatoid arthritis (RA) may occur through reduced myocardial mass rather than hypertrophy, and both modifiable and non-modifiable factors may contribute to lower levels of left ventricular mass and volume.14
Myocardial Ischaemia
CMR can detect ischaemia by two different ways:
Stress perfusion CMR has already been used for the evaluation of diabetic patients. In T1DM, myocardial perfusion reserve index (MPRI) was independently associated with increased LV torsion.28 In another study, it was documented that young subjects with uncomplicated T1DM have impaired myocardial energetics, irrespective of the duration of diabetes and the impaired cardiac energetics status results from metabolic dysfunction rather than microvascular impairment.29
Finally in a study by our group, adenosine stress CMR, using MPRI evaluation, detected early perfusion changes in asymptomatic T1DM, missed by the usual non-invasive evaluation.30
Stress perfusion CMR has also been applied in multisystem (rheumatic diseases). A 44 % prevalence of abnormal stress myocardial perfusion by CMR in the absence of obstructive CAD was documented in systemic lupus erythematosus (SLE) patients with anginal symptoms. Compared with controls, reduced MPRI was observed in SLE patients and SLE presence was a significant predictor of an abnormal MPRI. These findings are consistent with the hypothesis that anginal chest pain (CP) in SLE patients without obstructive CAD is due to myocardial ischaemia potentially caused by microvascular coronary dysfunction.31 Stress myocardial perfusion abnormalities were frequent in RA patients without known cardiac disease. Abnormal CMR perfusion findings were associated with higher RA disease activity, suggesting a role for inflammation in the pathogenesis of myocardial involvement in RA.32 Subclinical myocardial involvement, as detected by stress perfusion CMR, was frequent in asymptomatic patients with systemic sclerosis (SSc).33,34 Finally, in sarcoidosis without cardiac symptoms and normal routine assessment, stress perfusion CMR and myocardial inflammation assessment detected early cardiac involvement that may in some cases necessitate immediate treatment.35
Myocardial Viability (Fibrosis Detection or Viability Study)
Late Gadolinium Enhanced Imaging
CMR is the most reliable imaging way to detect and quantify scar or fibrotic tissue, due to irreversible myocardial damage (viability study). Following acute ischaemic injury, the myocardial distribution volume of gadolinium is increased due to sarcolemmal rupture and abnormal wash-out kinetics. The preferred imaging time for scar detection is between 10 and 20 minutes after contrast agent administration, when the differences between scar, normal myocardium and blood pool are maximal. This method is referred in the literature as late gadolinium enhanced (LGE) CMR and is the gold standard for the in vivo assessment of myocardial scar (see Figure 1). CMR can detect infarction in as little as 1 cm3 of tissue, substantially less than other in vivo methods, such as echocardiography and nuclear techniques. Furthermore, CMR can detect subendocardial myocardial infarction, missed by SPECT/PET. The CMR extent of scar predicts the potential for functional recovery after revascularisation.36–38
Subendocardial and/or transmural LGE, following the distribution of coronary arteries, are indicative of CAD. However, not only the presence but also the LGE amount plays an important role in patients’ prognosis, because even a small area of LGE (<2 % of LV mass) was associated with a greater than seven-fold increase in risk for a major adverse cardiac event.39
CMR can characterise silent scar consistent with myocardial infarction (MI) in diabetic patients without clinical evidence of MI, and has strong association with major adverse cardiovascular events (MACE) and mortality hazards that is incremental to clinical, electrocardiogram (ECG) and LV function combined.40
LGE has already been described in vasculitis, myositis, SLE and RA; it may present different patterns including subendocardial or transmural lesions in the territory supplied by the occluded coronary artery, intra-myocardial or subepicardial not following the distribution of coronary arteries, mimicking the pattern of viral myocarditis and/or diffuse subendocardial pattern due to vasculitis.41
Finally, global subendocardial LGE was identified by CMR in severe cardiac amyloidosis.42