Diabetes Mellitus Treatment – Interaction with Heart Failure
Glycaemic control is of importance in DM subjects with HF as it is supposed to decrease free fatty acid oxidation by myocardial cells and increase the use of glucose as a substrate for metabolic requirements.57 Nevertheless, attention must be given to the results of the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) and Action to Control Cardiovascular Risk in Diabetes (ACCORD) trials, which have shown that intensive treatment with a glycated haemoglobin target ≤6.5 % failed to influence macrovascular complications.58,59 The glycaemic control can be achieved with glucose lowering drugs of different categories and it seems that there are differences in the way that they affect HF. Nevertheless, most data are based on observational studies. Randomised control trials exist only for thiazolidinediones.
Thiazolidinediones
Thiazolidinediones are peroxisome proliferator-activated receptor gamma (PRARγ) agonists, which can induce sodium retention and HF. This effect results from the increase in tubular sodium and water reabsorption in specific nephron segments or from stimulation of sodium reabsorption in the collecting duct.60 Although PRARγ remains an attractive target for glycaemic control, thiazolidinediones’ clinical use is now limited and are avoided in patients with HF.71 Nevertheless, several non-thiazolidinedione selective PPARγ modulators free of sodium retention are now tested in preclinical trials.61
Incretins
Glucagon-like peptide-1 (GLP-1) agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors are a new class of anti-diabetic drugs. Except from their favourable effects in glycaemic control, preclinical data and early clinical reports support their clinical benefit in HF patients. GLP-1 increases cyclic adenosine monophosphate in cardiac myocytes but independently from a toxic increase in calcium levels and in myocytes xsxs.72 Preclinical data in dogs and pigs with dilated cardiomyopathy have demonstrated that infusion of GLP-1 improves left ventricle function and stroke volume.62,63 After myocardial infarction infusion of GLP-1, patients with left ventricle dysfunction showed improved ejection fraction and wall motion.73 A non-randomised study in 12 HF patients concluded that chronic infusion of GLP-1 significantly improves left ventricular function, functional status and quality of life in patients with severe HF.64 In contrast, Halbirk et al. concluded that 48 hours infusion of GLP-1 had no major cardiovascular effects in patients without diabetes but with compensated HF.74 Taken together we can conclude that although there are no definite data on the impact of incretins in HF, early observations favour their use in HF subjects.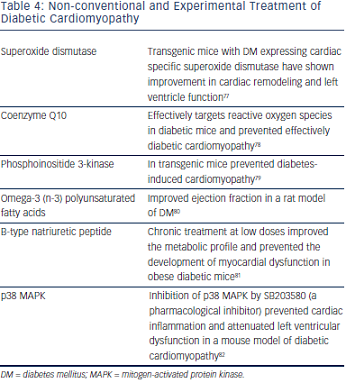
Other Glucose Lowering Treatment
The main concern regarding the use of metformin in HF patients despite their clinical benefits and the lower rates of mortality was the risk of lactic acidosis.65 Novel data do not support this risk.66,75 UK Prospective Diabetes Study (UKPDS) concluded that there was no difference between sulphonylureas and insulin treatment in cardiovascular complication,66 while it seems that metformin compared with sulphonylureas decrease hospitalisations at least in some studies.66,76 Regarding insulin treatment there are no reports that can affect HF status.67
Non-conventional Treatment of Diabetic Cardiomyopathy
Beyond the standard HF treatment, several novel approaches have been developed (see Table 4).
Ex vivo studies support the notion that superoxide dismutase can offer protection from HF.83 In vivo studies in transgenic DM mice expressing cardiac specific superoxide dismutase show improvement in cardiac remodeling and left ventricle function.77
Coenzyme Q10 is a potent antioxidant free of adverse effects, which can maintain cardiomyocyte and mitochondrial function. Recent preclinical data suggest that chronic supplementation with coenzyme Q10 can represent an effective approach for managing diabetic cardiomyopathy.78,84
Phosphoinositide 3-kinase is a cardioprotective kinase, which when enhanced in transgenic mice can prevent diabetes-induced cardiomyopathy adverse cardiac remodeling and dysfunction.79
Interestingly, numerous, mostly preclinical, studies have shown that interventions such as omega-3 (n-3) polyunsaturated fatty acids can improve cardiac output and ejection fraction as well as stroke volume and stroke work in a rat model of DM.80 This improvement may be mediated through attenuation of myocardial connexin-43 abnormalities. In contrast n-6 polyunsaturated fatty acids could accelerate myocardial abnormalities in diabetic rats.85