The Clinical Problem
The main physiological foundation of FFR is that it can only make inferences about the haemodynamic significance of a stenosis under conditions of maximal hyperaemia.6,7 Superficial interpretation of this presumption has led some to believe that the haemodynamic significance of a stenosis can only be assessed during maximal hyperaemia.8–10
This has significant clinical and physiological implications that have directly impacted the adoption of FFR and simultaneously hindered the development of novel indices.7
Clinically, hyperaemic agents such as adenosine cannot be administered to all patients, almost always cause patient discomfort and their administration adds significant time to the procedure. Even in the most practiced hands, in institutions that routinely perform physiological measurements, an FFR assessment has been shown to add at least 10 minutes to the diagnostic procedure.11
Scientifically, the overly simplistic assumption that a single dose of adenosine can achieve maximal hyperaemia in every single patient regardless of myocardial territory and co-morbidity is now coming under increasing scientific scrutiny. A plethora of factors can influence the degree of hyperaemia achievable, including the dose of hyperaemic agent, its route of administration, left ventricular end diastolic pressure, right atrial pressure, age, gender, concomitant medication, diet and even the sleep pattern of the patient.12–20
Physiologically, it is increasingly evident that maximal hyperaemia is impossible to achieve in the catheter lab and given the sheer number of variables affecting hyperaemia isolating the patients in which hyperaemia has been insufficient is equally impossible.21–23
This is particularly true of pressure-derived hyperaemic indices, such as FFR, which by definition do not measure flow and are therefore most vulnerable to this limitation.
This uncertainty has led clinicians to administer ever-increasing doses of adenosine and even adding other drugs to try and reassure themselves that ‘maximal hyperaemia’ is achieved. However, this only serves to create confusion because the FFR treatment threshold of 0.8 had not been validated against ischaemia at higher doses of adenosine making interpretation of the FFR value challenging and importantly not supported by outcome data. All these factors contribute to the poor ‘usability’ of FFR in the clinical domain – reflected in single figure adoption rates for FFR across most of the world despite a wealth of evidence being established for over 20 years.3
Can the Lessons of the Past Help us Find a Solution?
In recognition of the above limitations of FFR, hyperaemia-free indices have been introduced.4,5 These indices aim to circumvent the myriad limitations created by the need for administrating a hyperaemic agent in the hope of facilitated adoption by making procedures quicker, cheaper, safer and independent of the variability of attaining maximal hyperaemia. The most validated hyperaemia free index is iFR.4
iFR is not dependent on maximal hyperaemia and therefore shifts the paradigm away from maximal hyperaemia for the assessment of stenosis severity. This is based on a wealth of physiological data over the last 30 years that has clearly demonstrated that maximal hyperaemia is not required if stenosis assessment is made during a specific phase of the cardiac cycle.24–26
In a seminal experiment by Gould in 1978 it was demonstrated that the haemodynamic significance of stenoses could in fact be determined under basal conditions.24 Using combined pressure and flow velocity analysis he identified a phase in the cardiac cycle during which stenoses could reliably be differentiated into mild, moderate and severe. Using meticulous manual post hoc analysis of pressure and flow data he clearly demonstrated that the optimal period of the cardiac cycle to assess a 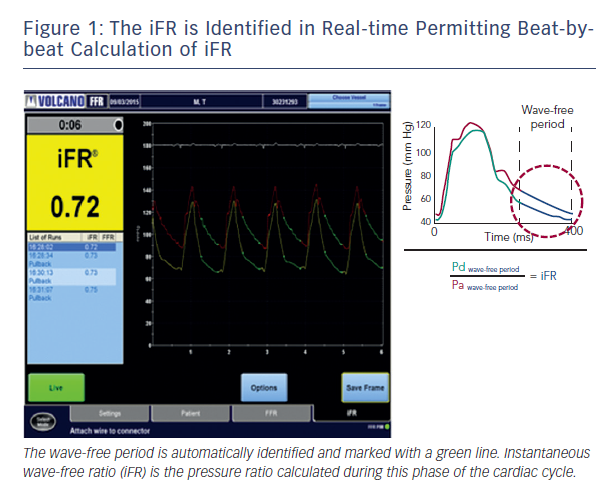
Recently, using combined pressure and flow assessment in humans wave intensity analysis identified a period within diastole when intra-coronary haemodynamics are also free of all wave activity, which is caused by relaxation and contraction of the myocardium.4 More importantly, using sophisticated computational algorithms this period can now be isolated in real-time on a beat-to-beat basis using the pressure waveform alone; making clinical use of this period feasible in daily clinical practice. It is during this period that iFR is calculated4 (see Figure 1).
Given the well-documented physiology of this period of the cardiac cycle and its unique suitability for stenosis assessment it is not surprising that iFR has been found to be able to determine the haemodynamic significance of stenoses. Furthermore because iFR can be measured within seconds, does not require hyperaemic agents and uses existing pressure wire technology its potential to improve adoption of physiology to realise the clinical and economic benefits of physiologically guided revascularisation is clear.28