iFR Validation Studies to Date
The classification match of iFR to FFR has been studied in over 3,500 vessels, this series of studies has definitively identified a treatment threshold of <0.9 for iFR.4,29–36
The agreement of iFR 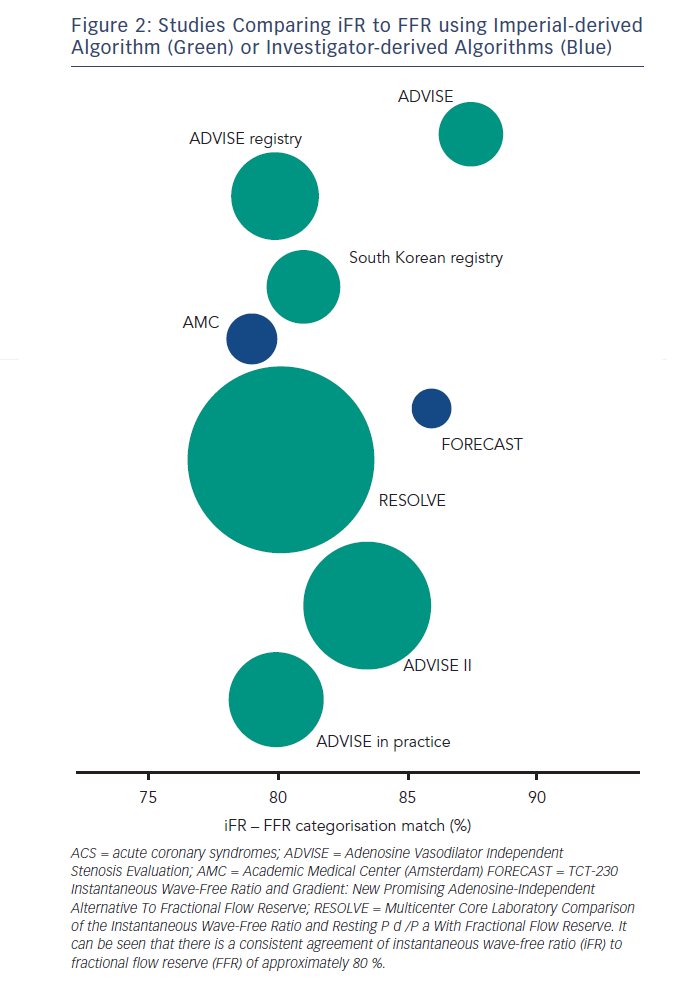 to FFR in the above studies has consistently been found to be approximately 80 % depending on the distribution of stenoses in the study population (see Figure 2). Interpretation of this statistic should take account of the fact that the classification match of two FFR measurements across the same lesion is not 100 % but 85 %.37,38 A finding suggested by the DEFER study39,40 but recently confirmed using modern pressure wire technology.41
to FFR in the above studies has consistently been found to be approximately 80 % depending on the distribution of stenoses in the study population (see Figure 2). Interpretation of this statistic should take account of the fact that the classification match of two FFR measurements across the same lesion is not 100 % but 85 %.37,38 A finding suggested by the DEFER study39,40 but recently confirmed using modern pressure wire technology.41
Such classification agreement between two FFR measurements across the same lesion is not surprising given the biological variability of any physiological measurement especially if that measurement is reliant on the heterogeneous and unpredictable effects of a hyperaemic agent.42
While FFR is viewed as a clinical standard for ischaemia it is widely accepted that there is no true gold standard test for ischaemia.43 Therefore, when two indices such as iFR and FFR agree so closely how do we interpret the significance of stenoses when iFR and FFR disagree? Several studies have attempted to look at this (see Figure 3).23,36,42–45 Each has taken iFR and FFR and compared with another index of stenosis severity. The salient findings of this body of research in over 500 stenoses are clear:
1. When iFR and FFR disagree – FFR is not necessarily correct.
2. Hyperaemia does not improve diagnostic accuracy.
The Joined Coronary Pressure and Flow Analysis to Determine Diagnostic Characteristics of Basal and Hyperemic Indices of Functional Lesion Severity-Coronary Flow Reserve (JUSTIFY-CFR) was the largest of these studies to systematically assess how iFR and FFR agree with underlying flow. It demonstrated that when iFR and FFR disagree that iFR was more indicative of the underlying flow characteristics of the vessel. Furthermore in the clinically relevant 0.6–0.9 FFR range, in which most of our patients fall, iFR was significantly more accurate than FFR.
Some have highlighted concerns with regards to the doses of hyperaemic agent, choice of reference test and therefore the validity of these studies. The meticulous validation of FFR during its development serves as template for the validation of new indices. It should be noted that FFR was validated against the same reference tests during its development,
using doses of adenosine and routes of administration identical to the studies now comparing iFR with FFR. Should we discount these pivotal FFR studies too? If so, what should be done with the guidelines and scientific recommendations supporting FFR that were based upon these?
The above studies clearly challenge the dogma that hyperaemia is necessary for stenosis assessment but also point to major potential differences between iFR and FFR that may make iFR more clinically useful than FFR.
Indeed the ability of iFR to be independent from the response of the microcirculation to a hyperaemic agent suggests that, it may also have a role in conditions that have traditionally been considered unsuitable for FFR assessment. The assessment of disease in the acute coronary syndrome population, vessels with tandem lesions, patients with renal failure, diabetes and hypertension are all vulnerable to a variable response of the microcirculation to hyperaemic stimuli – a limitation circumvented with resting indices. The role of iFR and FFR in these populations will be further elucidated in the Functional Lesion Assessment of Intermediate Stenoses to guide Revascularisation (DEFINE-FLAIR) and iFR SWEDEHEART studies.