Integrating Physiology into the DNA of Revascularisation – A Blueprint for the Future
To date, FFR has generally been used in a binary fashion to inform the clinician if th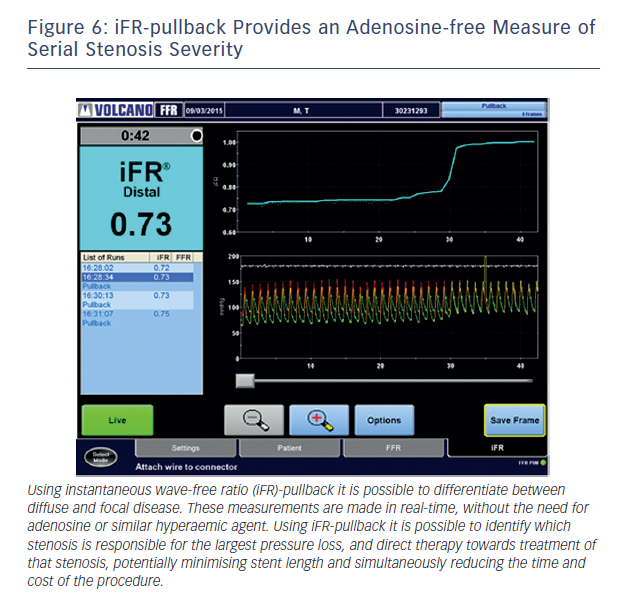
 CI by ensuring that
CI by ensuring that
the correct lesion is targeted.
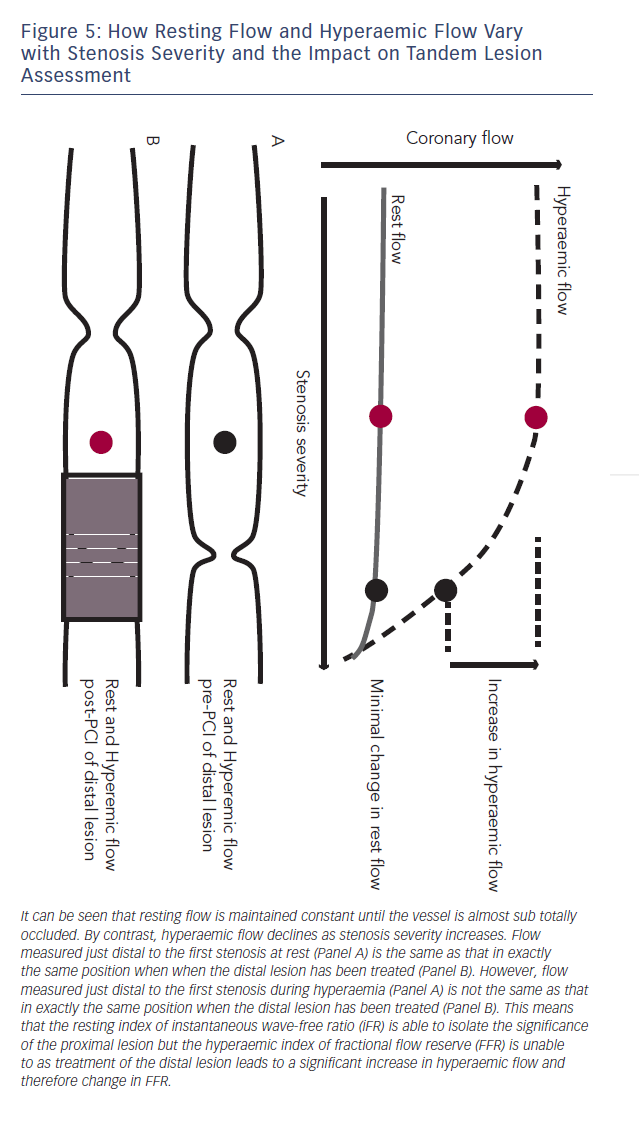
The reliance of FFR on maximal hyperaemia has prevented it from being used to isolate individual stenosis severity in vessels with tandem lesions.45,46 This is because when trying to assess the significance of a proximal stenosis the distal stenosis will blunt hyperaemic flow across the proximal lesion, therefore placement of the pressure sensor in between the two stenoses will under-estimate the severity of the proximal lesion. When the distal lesion is treated, hyperaemic flow is much higher and the FFR of the proximal vessel significantly different (see Figure 5).
Baseline indices, by contrast, are uniquely suited to the isolation of a specific stenosis in the context of tandem lesions. This is due to the fact that baseline flow is maintained constant until stenosi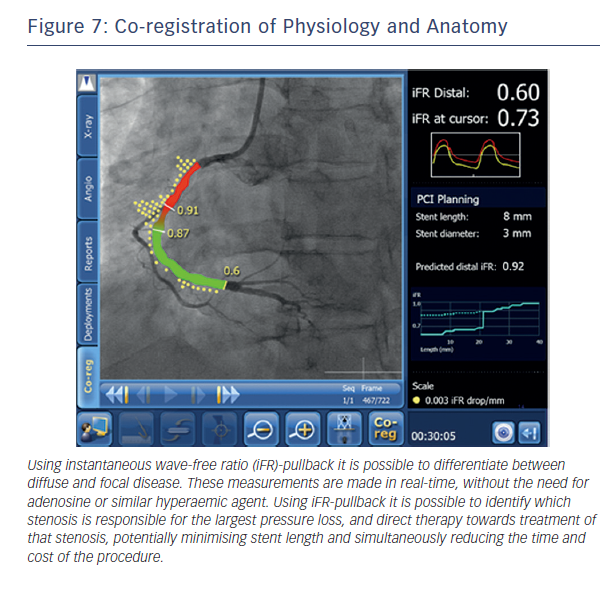
This ability to predict post-PCI iFR provides the potential to extend the role of physiology in interventional cardiology. Rather than simply informing us that a vessel is ischaemic, real-time hyperaemia-free point-to-point calculation of iFR along the entire vessel combined with co-registration with imaging will permit the possibility of virtual PCI. The clinician will therefore be able to determine (i) if a stent is required (ii) where the stent should be placed and (iii) the length of the stent to get the best haemodynamic result within a matter of seconds and remove the need for multiple hyperaemic pullback runs (see Figure 7).
Such an approach can be expected to significantly reduce stent length, procedural time and costs while simultaneously improving adoption in a patient population that is currently poorly served by FFR.