Fractional Flow Reserve
FFR assesses the physiologic significance of a coronary stenosis by calculating the ratio of distal coronary pressure (Pd) to proximal coronary pressure (Pa) during hyperemia.4 Coronary flow (Q) can be determined during maximal hyperemia with the coronary pressure measurement (Pa/Pd). The venous pressure (Pv) and the resistance of the myocardium (R) remain constant. By virtue of the physiology behind FFR measurement, attributes such as the extent of a perfusion territory, myocardial blood flow and the presence or absence of inducible ischemia are taken into account in evaluating stenosis severity.
How to Induce Maximal Hyperemia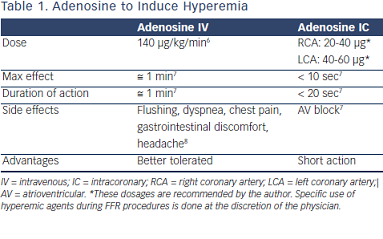
Multiple agents can be used to induce maximal hyperemia. The author prefers the use of intravenous (IV) adenosine, 140 μg/kg/min (Table 1). Papaverine is no longer favored, and nitroprusside has shown promise in several small trials.5
IV adenosine administered via a central (femoral) vein has been compared with an antecubital (peripheral) vein. The mean FFR difference between these IV infusion access routes at 140 μg/kg/min, although statistically significant, was only 0.0126.9 The author believes that experienced operators have a preference for IV adenosine due to the more reliable hyperemia state and fewer artifacts seen due to drug administration. Additionally, use of adenosine enables the operator to perform pullbacks for diffuse disease and provides the ability to easily disengage a catheter during FFR measurements of ostial disease.
How Reproducible is FFR? What is the Sensitivity and Specificity of FFR?
Multiple evaluations have shown the reproducibility of FFR measurements despite changes in loading conditions. In fact, serial evaluations have demonstrated the reproducibility of FFR measurements with the use of chronotropic and inotropic agents and afterload reducing agents.10,11 In a landmark study, Pijls et al. demonstrated that the sensitivity of FFR is 88 % while the specificity is 100 %.12
FFR and Microvascular Disease
It is known that multiple factors determine the functional severity of a stenosis in addition to the stenosis itself, including the extent and distribution of the perfusion territory, the state of the myocardium and the presence or absence of collaterals. The presence of microvascular disease can definitely be a confounder in the diagnosis and treatment of ischemic lesions and may contribute to a finding of reversible ischemia. FFR, however, can still indicate the contribution of an epicardial stenosis to the degree of inducible ischemia in patients with microvascular disease. FFR will show the exact maximum flow that can be achieved by removing the epicardial stenosis. Although coronary flow reserve (CFR) has been traditionally used to diagnose the presence of microvascular disease, measuring FFR can provide valuable information in these patients. Details regarding the validation of this concept have been presented elsewhere and are worthy of discussion.13 The evaluation of 150 lesions, with both FFR and CFR, found agreement between outcomes of FFR and CFR in 109 lesions (73%), and discordant outcomes in 41 lesions (27%). In 26 of these 41 lesions, FFR was < 0.75 and CFR ≥ 2.0. In 15 of these 41 lesions, FFR was ≥ 0.75 and CFR < 2.0.13 Concordance between CFR and FFR is seen in patients where FFR and CFR are normal and where FFR and CFR are abnormal. Cases where CFR is normal and FFR is abnormal are of concern. In this small subgroup of individuals, higher CFR levels fail to show the significance of a stenosis, which is evident with an abnormal FFR. Another group, and perhaps the most important, is that of patients with microvascular disease who have an abnormal CFR and a normal FFR. FFR fails to show the microvascular disease by virtue of the patient’s normal value. As a result, the lesion is not treated as the FFR is normal. The clinician arrives at the correct decision, despite the confounding information. In essence, FFR still determines accurately to what extent the maximum myocardial perfusion can be increased by coronary intervention.
The publication of this information was supported by St. Jude Medical.