Anatomic Evaluation with Optical Coherence Tomography
Optical coherence tomography (OCT) is an advanced imaging technique that enables ultra-high resolution evaluation of crosssectional biological systems. The near-infrared light source used in OCT allows for the evaluation of coronary artery disease (CAD) and vessel characteristics enabling PCI guidance with 10 times the resolution of IVUS.32 For this reason, previously difficult to image neointimal hyperplasia, fibrous caps or more sub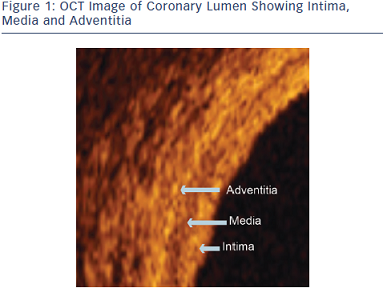 tle atherosclerosis can be seen with OCT.32 This allows for better visualization of the lumen, intima, media and adventitia where coronary pathology requiring evaluation is most prevalent (Figure 1).
tle atherosclerosis can be seen with OCT.32 This allows for better visualization of the lumen, intima, media and adventitia where coronary pathology requiring evaluation is most prevalent (Figure 1).
OCT Imaging Technique
The automated OCT system allows for a 75 mm pullback (survey mode) and 54 mm pullback (high resolution mode) after contrast administration at the level of the coronary vessel being evaluated via an automatic injector or manual injection. Mastering the technique for optimal OCT image acquisition is relatively easy. To minimize artifact, a 6 F catheter is recommended. A coaxial position with the catheter nicely engaged in the coronary artery is ideal. Predilatation of lesions may be necessary. Artifacts seen with OCT can include residual blood in the vessel lumen or swirl; blood inside the probe; nonuniform distortion; fold over, saturation or sew-up artifact; and Z-offset drift. All of these artifacts are relatively uncommon with the exception of residual blood in the lumen and blood inside the probe. The first one is easily remedied with better contrast injection, and the second one by simply flushing the OCT catheter.
Angiography and OCT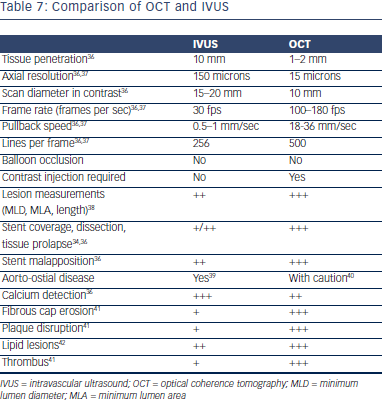
The limitations of angiography in the evaluation of CAD were previously discussed. When comparing angiography alone with angiography plus OCT to guide decision-making during PCI, the CLI-OPCI study suggests that the use of OCT can improve clinical outcomes of patients.33 Though an observational study with obvious limitations, it is nonetheless hypothesis generating and is the first study suggesting a direct relationship between the use of OCT and a clinical outcome. OCT found adverse features requiring further interventions in 34.7 % of cases. The unadjusted analysis showed that the OCT group had a significantly lower 1-year risk of cardiac death, MI or repeat revascularization (9.6 % vs. 14.8 %, p=0.044). OCT did not increase short-term or mid-term adverse events demonstrating proof of its safety. The statistically significant reductions in cardiac death or nonfatal MI suggest that OCT guidance may minimize procedural issues, particularly periprocedural and in-hospital MI.33
IVUS vs. OCT
Both IVUS and OCT can be used to visualize minimum lumen diameter (MLD), MLA, lesion length, calcium, fibrosis and lipids. However, when it comes to evaluation of strut apposition, stent coverage, cap fibroatheroma evaluations, thrombus and macrophages, OCT tends to be better by virtue of the higher resolution. Post-intervention findings such as dissection, tissue prolapse and apposition tend to be seen better with OCT.34,35 Table 7 compares attributes and charact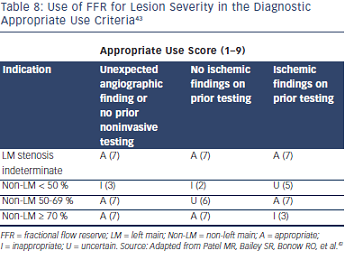 eristics of IVUS and OCT.
eristics of IVUS and OCT.
FFR and OCT
There is a benefit to integrating FFR and OCT technologies for the evaluation of disease and PCI optimization. These tools offer physicians the ability to identify, diagnose and treat CAD while improving outcomes. FFR is considered the gold standard in the detection of myocardial ischemia and enables high-fidelity hemodynamic and physiologic evaluation. FFR has been shown to improve outcomes in the treatment of multivessel disease as evident by the results of the FAME 1 study. FFR also enables evaluation of multiple other lesion subsets that could facilitate interventional procedures. See Table 8 for appropriate use criteria.43
OCT represents a leap in intravascular imaging and provides superior resolution when compared with IVUS. Advanced imaging enabled by OCT facilitates procedural decisions and may result in improved outcomes. Specifically, OCT allows for better plaque characterization and superior evaluation of post-interventional results and facilitates research endeavors requiring high resolution.
The publication of this information was supported by St. Jude Medical.