FFR in Ostial Disease and Jailed Side Branches
Ostial disease often represents a challenge in the interventional treatment of coronary disease. Lesion location and characteristics may make it difficult to stent ostial lesions while trying to preserve the parent vessel that is disease-free. Most side branch lesions and ostial d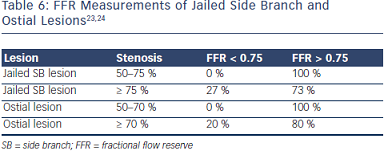 isease do not have functional significance, and quantitative coronary angiography is unreliable in assessing the functional severity of these lesions.23, 24 However, various studies have shown the ability of FFR to clearly evaluate these lesions (Table 6).23, 24
isease do not have functional significance, and quantitative coronary angiography is unreliable in assessing the functional severity of these lesions.23, 24 However, various studies have shown the ability of FFR to clearly evaluate these lesions (Table 6).23, 24
FFR in Acute Coronary Syndromes
Questions have been raised as to the value and safety of FFR in the setting of acute coronary syndromes (ACS). It is standard practice to avoid measuring FFR in an infarct-related artery and territory until after 5 to 7 days. However, FFR in a non-infarct-related artery or other territories can still be evaluated in the acute setting as long as it is clinically safe and required. The benefit of using FFR to guide percutaneous coronary intervention (PCI) in multivessel disease does not differ in patients with unstable angina (UA) or non-ST-segment elevation myocardial infarction (NSTEMI) compared with patients with stable angina.25
What Do the DEFER, FAME 1 and FAME 2 Studies Show About FFR?
Assessing individual coronary lesions in an effort to find if they are responsible for ischemia has important prognostic implications. The DEFER study is a prospective, randomized, multicenter study that evaluated lesion significance with FFR (< 0.75) and followed patients for future events. The 5-year follow-up of these patients demonstrated that event-free survival was similar for patients with or without interventions at FFR > 0.75.26 Medical treatment of patients with a hemodynamically nonsignificant stenosis (FFR > 0.80) in the proximal left anterior descending artery (LAD) is associated with an excellent long-term clinical outcome with survival at 5 years similar to an age-related and sex-matched control population.27
The routine measurement of FFR during PCI with drug-eluting stents in patients with multivessel disease was compared with a strategy of angiography alone in the FAME 1 study. The study demonstrated an approximate 30 % reduction of the composite endpoint of death, myocardial infarction (MI), revascularization and bypass at 12 months. It also showed that the FFR-guided strategy resulted in cost saving, did not prolong the procedure, reduced the total numbers of stents used, decreased the amount of contrast used and resulted in a similar, if not better, functional status. The results of FAME 1 support the paradigm of a “functionally complete revascularization” by stenting only the significant lesions and medically treating nonsignificant lesions.28-30
The FAME 2 study compared FFR-guided PCI plus optimal medical therapy (OMT) versus OMT alone. The primary endpoint was a composite of death, MI and urgent revascularization. FAME 2 was halted prematurely as events favored PCI plus OMT. The results were largely driven by urgent revascularization (1.6 % vs. 11.1 %). In patients with stable CAD, PCI plus OMT decreased the need for urgent revascularization when compared with OMT alone. In essence, FFR may identify stable CAD patients who may fare worse with OMT alone.31
The publication of this information was supported by St. Jude Medical.