Coronary Physiology vs. Coronary Anatomy (Intravascular Imaging/Angiography)
The interventional community has long used intravascular imaging to answer the physiologic question of lesion significance (ischemic vs. nonischemic). While validation studies may have shown some correlation between intravascular imaging and the ischemic significance o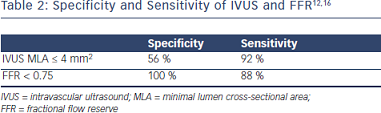 f a lesion, this diagnostic modality has its obvious limitations. There is a known discordance between FFR and intravascular ultrasound (IVUS) when it comes to lesion significance.14, 15 As such, physiologic questions require a physiologic answer, while anatomical questions require an anatomical answer (Table 2).
f a lesion, this diagnostic modality has its obvious limitations. There is a known discordance between FFR and intravascular ultrasound (IVUS) when it comes to lesion significance.14, 15 As such, physiologic questions require a physiologic answer, while anatomical questions require an anatomical answer (Table 2).
This should not be surprising as multiple physiologic measures of a lesion’s significance cannot be evaluated with an anatomical evaluation. Evaluation of a single cross-sectional area (CSA) does not take into account the lesion entrance effect, friction-derived loss of pressure, flow separation losses, blood viscosity and lesion turbulence. Moreover, the inherent value of a vessel’s myocardial distribution (small or large) and the condition of the myocardium (microvascular disease or not) must be evaluated physiologically not anatomically. Therefore, the limitations of an anatomical evaluation should not be surprising. A similar limitation may exist when comparing myocardial perfusion imaging with FFR.17
Recent studies have also shown the direct relationship between IVUS and FFR for a given vessel size. The FIRST trial (Fractional Flow Reserve and IVUS Relationship Study) s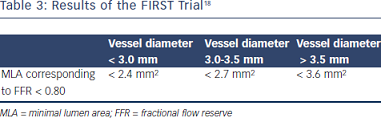 howed 64 % sensitivity and a 65 % specificity finding that a minimum lumen area (MLA) > 3.07 corresponded to a FFR < 0.80.18 The accuracy of IVUS improved when a reference vessel analysis was performed (Table 3).18
howed 64 % sensitivity and a 65 % specificity finding that a minimum lumen area (MLA) > 3.07 corresponded to a FFR < 0.80.18 The accuracy of IVUS improved when a reference vessel analysis was performed (Table 3).18
The inherent limitations of angiography also provide the basis for some subjectivity in the evaluation of ischemic lesions. The limitations on revascularization decision making can be seen in a comparison of FFR and angiographically guided evaluation on lesion significance during routine assessment (Table 4).19
The limitations of angiography and IVUS in identifying intermediate lesions able to produce ischemia have led contemporary interventional cardiology to call for more advanced and reliable means of evaluating lesion significance. FFR has been able to change that paradigm.
FFR in Diffuse Disease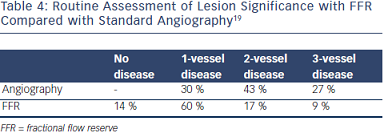
Diffuse disease represents a challenge in the evaluation of significant lesions. Often, tandem lesions may not look significant on angiography but may have a physiologic impact in combination. IVUS may not identify a significant minimal CSA or MLA among the tandem lesions. It is also challenging to find reference segments when diffuse disease is present. FFR provides the ability to evaluate the significance of those lesions. It also allows for a pullback (with the use of IV adenosine), which can be helpful in identifying delta changes that unmask the significance of one lesion versus another. FFR provides for great spatial resolution. Lesions with the largest significant gradient are treated first. Subsequent FFR evaluations will be able to reveal if the remaining lesions are still ischemia producing or not.
FFR vs. Intravascular Imaging in Left Main Disease
The angiographic evaluation of left main (LM) disease is another situation that can present challenges and require additional intravascular imaging in order to make the correct decision regar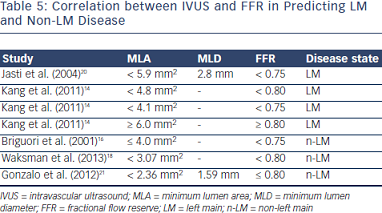 ding revascularization. The angle of the ostium in particular often presents challenges for the accurate angiographic evaluation of disease. Multiple validation studies have been performed to show the MLA at which severe disease is present (Table 5).
ding revascularization. The angle of the ostium in particular often presents challenges for the accurate angiographic evaluation of disease. Multiple validation studies have been performed to show the MLA at which severe disease is present (Table 5).
It is important to remember that when evaluating ostial LM disease one has to disengage the catheter from the ostium during pressure measurements. In this case, IV adenosine may facilitate the recording process. FFR evaluation of the LM is critically dependent not only on the lesion characteristics but also on the territory supplied by the vessel. In the hypothetical case that there is an area of infarct in the territory of a given vessel, the quantity of viable myocardium supported by the vessel will be reduced and the FFR could be higher. This is not to be considered an underestimation of the severity of the ischemia by FFR but simply that the lumen is adequate for the amount of viable myocardium present. Alternatively, the FFR may be lower when a given vessel also supplies the collateral flow to another vessel territory. In this case, the supplied territory for a given vessel has increased rendering of an otherwise insignificant lesion to become FFR positive. When comparing FFR and intravascular imaging in isolated LM disease, it seems that the MLA at which LM disease shows an FFR < 0.80 is < 4.8 mm2.14
Evaluation of LM disease in the presence of significant proximal disease of the left anterior descending and circumflex arteries is still controversial. A clinically relevant effect on the FFR assessment of LM disease with the pressure guidewire in a nonstenosed downstream vessel occurs only when the stenosis in the other vessel is proximal and very severe, as validated in an animal study.22 This means that FFR in the presence of isolated LM disease is very reliable. As a general rule, it seems to be accepted that an FFR in the LM < 0.8 or an MLA < 5.9-6.5 mm2 is the threshold for revascularization.
The publication of this information was supported by St. Jude Medical.