Embolisation of atherothrombotic material is a common occurrence during percutaneous coronary intervention (PCI) in ST-elevation myocardial infarction (STEMI). This may lead to distal vessel occlusion resulting in impaired myocardial perfusion, which is associated with larger infarct size, incomplete ST resolution and increased mortality. Unfortunately, there is a lack of significant adjunctive devices to protect the microcirculation. A symposium was sponsored by Inspire MD and chaired by Alexandre Abizaid, Institute Dante Pazzanese de Cardiologia (Sao Paulo, Brazil), and Jean Fajadet, Clinique Patteur, (Toulouse, France). These presentations aimed to discuss the importance of thrombus management in PCI for STEMI patients, to give an update of relevant clinical data on the performance of the MGuard™ stent in STEMI patients and to present real life examples on how this device selection can influence the outcome in STEMI patients.
Therapeutic Alternatives for Intracoronary Thrombus – MASTER Results in Perspective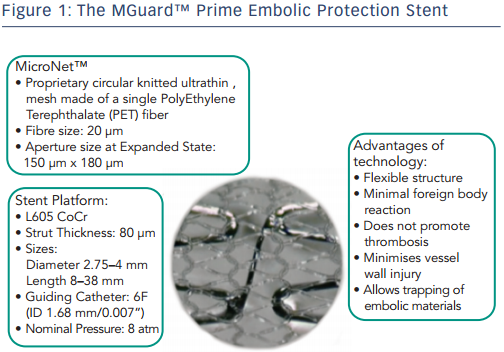
Alexandre Abizaid and Chaim Lotan
Dr Abizaid began by emphasising the need for therapeutic alternatives to avoid distal thromboembolism (embolisation) during highly thrombotic situations such as STEMI. The Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS), prospective randomised trial, aimed to determine whether aspiration of thrombotic material before stent implantation of the infarct-related coronary artery resulted in improved myocardial perfusion compared with conventional primary PCI.1 Results showed a reduction in all-cause mortality at 30 days. However, the Thrombus Aspiration during ST-segment Elevation myocardial infarction (TASTE) study (n= 7244) found that routine thrombus aspiration before PCI as compared with PCI alone did not result in a reduction in 30-day mortality.2 Even if aspiration is good, embolisation remains an ongoing issue.
The MGuard™ Embolic Protection Stent (EPS) is a novel device. The EPS has evolved from the stainless steel MGuard to the L605 cobalt chromium MGuard Prime, b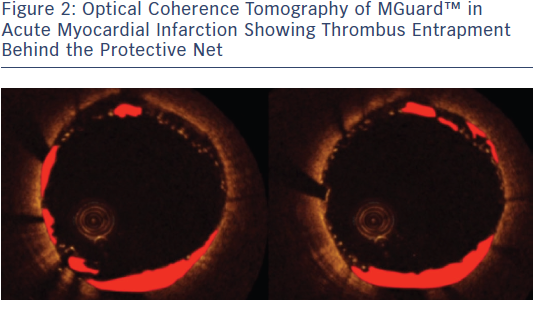 oth featuring a polyethylene terephthalate (PET) mesh with 150–180 μm aperture size, preventing the prolapse of thrombus and potential distal embolisation (see Figure 1). Case reports in patients with STEMI undergoing primary PCI have demonstrated the ability of the MGuard EPS to capture and contain (‘jail’) thrombus and atheroma behind its net, thereby preventing distal embolisation (see Figure 2).
oth featuring a polyethylene terephthalate (PET) mesh with 150–180 μm aperture size, preventing the prolapse of thrombus and potential distal embolisation (see Figure 1). Case reports in patients with STEMI undergoing primary PCI have demonstrated the ability of the MGuard EPS to capture and contain (‘jail’) thrombus and atheroma behind its net, thereby preventing distal embolisation (see Figure 2).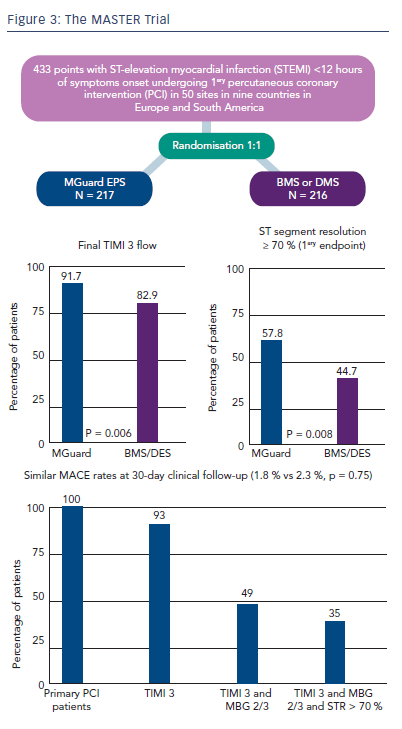
The MGuard for Acute ST Elevation Reperfusion (MASTER) trial recruited 432 patients with symptoms consistent with STEMI within 12 hours of symptom onset, at 50 sites in nine countries.3 Participants were randomised to PCI with bare metal stent (BMS) or drug-eluting stent (DES), (n=216) or to PCI with MGuard (n=217). Follow-up was at 30 days, six months and one year. The primary endpoint was ST-segment resolution at 60–90 minutes. Other inclusion criteria were ≥2 mm of ST-segment elevation in ≥2 contiguous leads and PCI of a single de novo lesion with reference vessel diameter (RVD) ≥3.0 to ≤4.0 mm and length ≤33 mm (capable of being covered by a single study stent). The primary endpoint of post-procedure complete (≥70 %) ST-segment resolution was significantly higher in the MGuard stent group compared with the control group (57.8 % vs 44.7 %; difference: 13.2 %; 95 % confidence interval: 3.1 % to 23.3 %; p=0.008; see Figure 3). The MGuard EPS also showed superior rates of thrombolysis in myocardial infarction (TIMI) 3 flow (91.7 % vs 82.9 %, p = 0.006).
Major adverse cardiac events (1.8 % vs 2.3 %, p=0.75) at 30 days were not significantly different between the two groups. Although the study was not powered for mortality, a trend in favour of the MGuard EPS was observed (0 % vs 1.9 %, p=0.06). A substudy, in which patients underwent magnetic resonance imaging (MRI) at five days, showed a trend towards smaller infarct size measured by delayed enhancement with the MGuard EPS.4 At 12 months, the trend towards reduced cardiac mortality with the MGuard EPS was still seen but again did not reach statistical significance (1.0 % vs 3.3 %, p=0.092).5 No significant differences in reinfarction or stent thrombosis were seen at 12 months between the MGuard EPS and control groups. The 12-month target lesion revascularisation (TLR) rate and 13-month late loss and binary restenosis rates for the MGuard EPS was higher than the in control group but comparable to other BMS cohorts such as in the large Harmonising Outcomes with RevasculariZatiON and Stents in Acute Myocardial Infarction (HORIZON) trial.4 Another subanalysis divided patients into two groups according to the measured volume of thrombus (≤ or >30 mm2). In the small thrombus group, complete resolution of ST-elevation was achieved in 66.2 % of the MGuard group vs 44.9 % of the control (p=0.02).6 In the large thrombus group, complete resolution was achieved in 54.7 % of the MGuard group vs 42.3 % of the control (p=0.02). These data suggest that the device may be successfully employed in patients with large thrombus burden.
In conclusion, among patients with STEMI undergoing emergent PCI, the MGuard EPS resulted in superior rates of restored flow (TIMI 3) and complete resolution of ST elevation, with a trend to reduced mortality compared with control groups.
The publication of this article was supported by InspireMD.