The Enemy of Primary PCI
Chaim Lotan
Dr Chaim Lotan, Hadassah Medical Center (Jerusalem, Israel) discussed the clinical challenge of ‘no-reflow’ in primar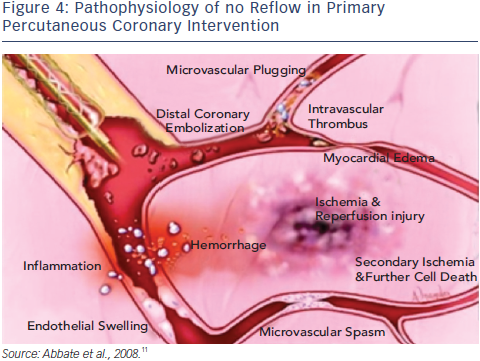 y PCI. Angioplasty is associated with improved epicardial flow, greater reperfusion rate and improved survival, when compared with thrombolytic therapy.7 However, despite TIMI 3 flow, optimal myocardial reperfusion is probably only achieved in one third of patients.8 This phenomenon is known as slow flow or no-reflow and characterised by ‘slow flow’ in the affected vessel and lack of contrast uptake (‘blush’) by the subtended myocardium, which is associated with a poor prognosis.9,10 The pathophysiology of no reflow is described in Figure 4.11 It is a multifactorial condition and is caused by four interacting mechanisms: ischaemic injury, reperfusion injury, distal embolisation and susceptibility of the microcirculation to injury.12 The timing of distal embolisation varies and can affect outcomes: distal embolisation before PCI is visible in 5 % of angiograms before PCI and in 15–17% after PCI.13,14 Thrombus composition and size is also related to outcomes. Fresh thrombus that can be aspirated typically only represents 30 % of the total thrombus load. The plaque represents 24 % and organised thrombus accounts for 47 %.15 Furthermore, angiography underestimates residual thrombus after aspiration; this can be demonstrated by optical coherence tomography (OCT).16
y PCI. Angioplasty is associated with improved epicardial flow, greater reperfusion rate and improved survival, when compared with thrombolytic therapy.7 However, despite TIMI 3 flow, optimal myocardial reperfusion is probably only achieved in one third of patients.8 This phenomenon is known as slow flow or no-reflow and characterised by ‘slow flow’ in the affected vessel and lack of contrast uptake (‘blush’) by the subtended myocardium, which is associated with a poor prognosis.9,10 The pathophysiology of no reflow is described in Figure 4.11 It is a multifactorial condition and is caused by four interacting mechanisms: ischaemic injury, reperfusion injury, distal embolisation and susceptibility of the microcirculation to injury.12 The timing of distal embolisation varies and can affect outcomes: distal embolisation before PCI is visible in 5 % of angiograms before PCI and in 15–17% after PCI.13,14 Thrombus composition and size is also related to outcomes. Fresh thrombus that can be aspirated typically only represents 30 % of the total thrombus load. The plaque represents 24 % and organised thrombus accounts for 47 %.15 Furthermore, angiography underestimates residual thrombus after aspiration; this can be demonstrated by optical coherence tomography (OCT).16
The MGuard EPS prevents post stenting protrusion of the remaining thrombus, commonly seen with conventional stent, as the micronet seals (“jails”) the thrombus against the vessel wall.
The publication of this article was supported by InspireMD.