Section A
Techniques for Chronic Total Occlusions Revascularisation
Device-Assisted Antegrade Dissection/Re-entry
The primary mode of failure when recanalising a chronically occluded vessel is entrapment of the guidewire and support equipment within the subintimal/subadventitial space and the inability to return into the distal true lumen. Recent technologies, “CrossBoss™” catheter, Stingray™ balloon and Stingray™ re-entry guidewire, Boston Scientific, (Natik, MA) have addressed this limitation and have provided a reproducible and systematic method for successfully gaining re-entry into the coronary lumen. The CrossBoss catheter is a metal-braided, over-the-wire, support catheter with a 1-mm rounded distal tip, which can be used to support standard guidewire manipulation or can be advanced using rapid rotation, with or without the wire lead. Without the wire lead, this catheter can cross into the distal true lumen of approximately 40 % of lesions.25 Alternatively it can enter into a side branch (which is important to recognise to avoid perforation) or cross within the subintimal space. This device’s relative safety and minimal perforation risk and the change in technique to a wire-skill independent model make it attractive for CTO crossing.25
If the CrossBoss catheter reaches a subintimal position, or if a standard wire strategy leads to subintimal wire entrapment, coronary re-entry can be systematically achieved with the Stingray coronary re-entry technologies (Boston Scientific). The Stingray balloon is a 1 mm thick, over-the-wire, balloon catheter with three exit ports (one distal and two 180°, diametrically opposed, side ports). When the balloon is inflated, it effectively wraps the artery with an exit port that is always directed towards the adventitia and an exit port that is always directed towards the lumen. Using fluoroscopy, operators can select the lumen port with the dedicated Stingray re-entry wire and achieve distal lumen control. Occasionally, subintimal wire entry can cause subintimal haematoma that can compress the distal true lumen, requiring aspiration through an over-the-wire balloon or microcatheter for decompression to enable distal true lumen re-entry (subintimal transcatheter withdrawal [STRAW] technique). For operators with access to these technologies and techniques, the need for the aforementioned parallel wire or wire-based re-entry methods is low. These technologies have been highly successful and have had low complication rates, even in early experiences and in refractory cases.25,26
The Retrograde Approach
In 2005, Katoh et al. pioneered the modern era of retrograde CTO recanalisation,27 by introducing the following new techniques – targeted septal or epicardial collateral crossing, retrograde lesion crossing and management of the subintimal space through the use of balloon dilation for connecting antegrade and retrograde channels.8 Currently, retrograde procedures account for 15–34 % of all CTO PCI procedures in European and USA registries.5,28–30 These methods require access to the distal CTO vessel from a collateral (or occasionally bypass graft) vessel with successful placement of a support catheter.31
Retrograde Wire Crossing
Retrograde wire crossing indicates lesion crossing in the distal to proximal cap direction with successful true lumen access to the proximal vessel.8 The standard approach after successful retrograde wire manipulation includes placing the wire and then the microcatheter into the antegrade guide catheter and then exchanging for a long wire to be externalised from the antegrade guide.32 The externalised wire, such as the ViperWire™ Advance (CSI, St Paul Minnesota), R350, Vascular Solutions (Minneapolis, Minnesota), RG3 (Asahi Intecc) is then used as the interventional platform to complete the PCI procedure.33 It is important for the retrograde guidewire to remain covered by a microcatheter to protect the collateral vessel from injury and to pay careful attention to guide movement to prevent guide-induced donor vessel injury.
Kissing Wire Technique
This technique combines the antegrade and retrograde approaches,34 although CTO penetration is achieved from the antegrade route. If the CTO lesion is relatively soft, the retrograde wire can be advanced easily, with the operator stopping the wire half way through the lesion. If the tip nears the CTO proximal cap, the operator can aim the tip towards the antegrade guide wire. Eventually, the antegrade and retrograde guide wires meet or “kiss”. This technique is generally used to reduce the use of contrast and to eliminate any potential ambiguity regarding the course of the vessel, thus making advancement of the antegrade wire safer. After crossing with the antegrade wire, the balloon catheter is advanced into the occlusion and dilatation is performed. The kissing wire technique is rarely performed by experienced retrograde operators, as the reverse controlled antegrade and retrograde tracking and dissection [CART], as described below) technique provides a more consistent method for connecting the channels in refractory cases.
Knuckle Technique35
In this technique a dissection of the subintimal space is created by forming a loop in the retrograde wire, which is then advanced into the occluded segment. For this technique, soft hydrophilic wires are preferred, especially if there is good support from the retrograde microcatheter, for example the Corsair channel dilator (Asahi Intecc). However, an antegrade stiff wire is generally required in order to pass through the dissected lumen created by the knuckle wire. After crossing with the antegrade wire, PCI is performed as per usual fashion.36
CART Technique37
The principle of this technique is to create a subintimal dissection with limited extension only at the CTO site, thereby facilitating antegrade wire crossing. In practice, this involves exchanging the microcatheter for a balloon catheter after septal collateral dilation with a Corsair catheter or a small balloon (however, epicardial collaterals should never be dilated). This balloon catheter is advanced retrograde into the lesion and overlapped with the antegrade equipment. Dilation with an appropriately sized balloon will typically create a connection between the antegrade and retrograde spaces, which can be subsequently wired. The main disadvantages of this method include the need to pass the wire into an often small and diffusely diseased distal lumen and the inability to effectively use intravascular ultrasound to optimise the strategy.
Reverse CART Technique
The principle behind this technique is the same as that of the CART technique, except that the connected space is created with antegrade balloon dilation (after overlapping with the retrograde catheter), thereby facilitating the crossing of the occlusion with the retrograde wire. Currently, this is the dominant technique in the retrograde CTO approach.29 The optimal wire position for reverse CART is when both the antegrade and retrograde guidewire are located within the subintimal space. The most common reason for failure of this technique is use of undersized balloons, that can be prevented by using intravascular ultrasound for optimal balloon sizing and positioning.38
The most common current methods for successfully completing a retrograde CTO PCI procedure are the “true” wire crossing with externalisation and the reverse CART with wire externalisation. The kissing wire technique, the knuckle technique (without adjunctive reverse CART) and the classic CART technique are included for review completeness but are rarely performed at present.29
Hybrid Strategy for CTO PCI
Contemporary antegrade, retrograde and dissection and re-entry techniques are complementary and necessary for the full spectrum of CTO PCI. Exploring sequential CTO crossing options can increase success, shorten procedural time and reduce radiation exposure. The CTO expert operator needs broad skillsets, versatility and flexibility to accommodate the wide range of anatomic scenarios for chronic occlusion that will be prese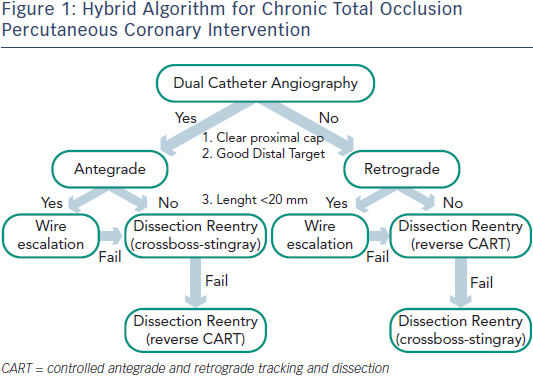 nt in patients with strong indications for revascularisation.39
nt in patients with strong indications for revascularisation.39
While significant variability exists with many operators with respect to procedural approaches, the “hybrid method” for CTO PCI represents an effort to standardise initial and provisional technique selection based on patient anatomy (see Figure 1).7 The implementation of the hybrid method requires skillset development in optimal wire manipulation, dissection/re-entry strategies and retrograde techniques. The development and adoption of only one or two of these skillsets will ultimately limit the experienced operator who wishes to approach all patients with appropriate indications for revascularisation. Failure to develop all three skillsets will likely lead to the dilemma of underutilisation of revascularisation in subgroups of patients who may derive the greatest benefit from these techniques.
Development of a CTO PCI Program
Successfully developing a CTO PCI program requires several steps; developing consensus among cardiologists (interventional and noninvasive), cardiac surgeons and hospital administrators regarding the rationale for CTO revascularisation; ensuring appropriate patient selection with individualised consideration of the risk/ benefit; obtaining CTO-specific didactic and hands-on training by experienced CTO operators; and establishing a quality assurance program with accountability of procedural results and acute and long-term clinical outcomes.40 The importance of the “heart team” that enables collaborative work between cardiac surgeons and cardiologists in making coronary revascularisation decisions for patients with complex coronary artery disease including CTOs, cannot be overemphasised.41
The authors would like to thank Ms Sheila Agyeman for her invaluable effort in coordinating the manuscript creation process.