Post-operative Care
Patients should have a temporary pacing wire in situ with cardiac monitoring for 24–48 hours after the procedure, as they are at risk of arrhythmias. High-grade AV block resolves in the majority of cases within three days.76 On discharge, patients should be 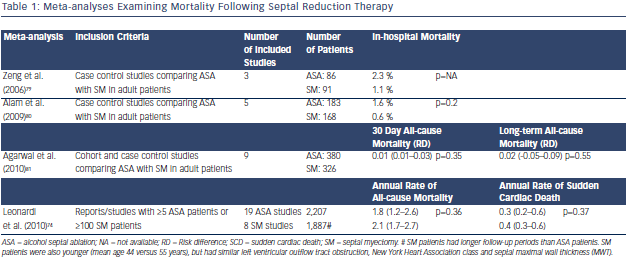 advised to report arrhythmic symptoms as rarely new onset bradyarrhythmias develop late after the procedure.77 Cardiac biomarkers peak at 12 hours post-ASA and correlate with the size of myocardial injury.78 In the absence of new conduction abnormalities, pharmacotherapy for symptomatic LVOTO should continue until a clinical review in 3–6 months, and can then be tapered if symptoms have improved.
advised to report arrhythmic symptoms as rarely new onset bradyarrhythmias develop late after the procedure.77 Cardiac biomarkers peak at 12 hours post-ASA and correlate with the size of myocardial injury.78 In the absence of new conduction abnormalities, pharmacotherapy for symptomatic LVOTO should continue until a clinical review in 3–6 months, and can then be tapered if symptoms have improved.
Long and Medium-term Outcomes– Alcohol Septal Ablation Versus Myectomy
Mortality associated with ASA and surgical myectomy has been examined and compared in four meta-analyses.74,79–81 Even though the meta-analyses included individual studies with very different inclusion criteria, they have consistently shown that the two procedures have similar survival outcomes (see Table 1). Both septal reduction therapies achieve similar improvements in symptoms, which is the principal aim of invasive therapy. However, myectomy is associated with a greater reduction in gradients and reduced need for post-procedural anti-bradycardia pacing (see Table 2).74,79–81 Concerns over the long term arrhythmogenic potential of the myocardial scar induced by alcohol septal ablation67 are not supported by observational data of implantable cardioverter defibrillator (ICD) recipients undergoing the procedure82 or mortality data from the meta-analyses.74,79– 81
Proced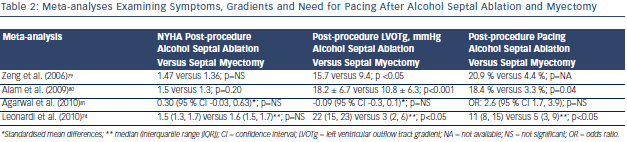 ural Failure
ural Failure
ASA is effective at reducing symptoms in more than 85 % of patients.69 In cases of procedural failure, defined by the persistence of both symptoms and LVOTO (rest or latent), further intervention with any of the modalities may be considered following a repeat assessment of the mechanisms responsible for symptoms. As changes in LV morphology following ASA may be delayed, it is prudent to delay decisions regarding further intervention for 3–6 months.83
Significant symptoms may persist in about 10–20 % of patients despite LVOTO abolition, illustrating the importance of the complexity of the disease and appropriate patient selection. It is therefore important to counsel patients that LVOTO reduction does not cure HCM and ongoing care will be required to monitor and treat their disease.
Alternative Percutaneous Septal Reduction Therapies
Alternative approaches to reduce hypertrophy at the point of mitral-septal contact by means other than alcohol have been investigated:
Experience with these alternatives is limited and long-term safety data are not available.
Care Beyond Left Ventricular Outflow Tract Obstruction
LVOTO should not overshadow other aspects of management; patients in whom LVOTO is successfully abolished are still subject to other HCM-related risks and outcomes. HCM should be evaluated in units with relevant expertise to address family screening and genetic testing, the risk of sudden cardiac death, atrial arrhythmias and prevention of stroke.