Summary
Scenario I – In-stent Restenosis
In-stent restenosis (ISR) is a major clinical problem faced in the cath lab. OCT has the capacity to differentiate ISR from 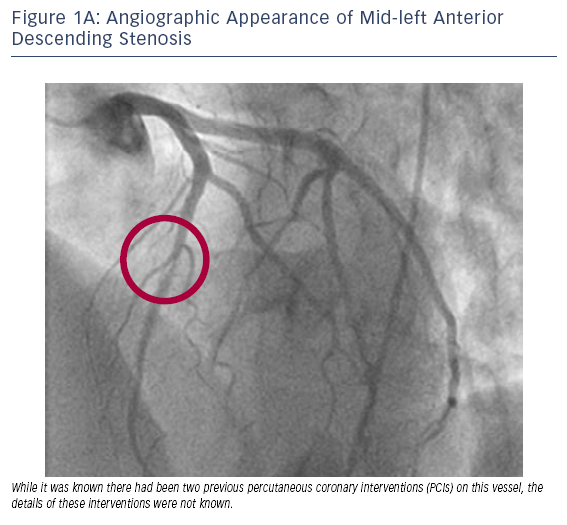 other pathologies and can easily distinguish stent struts. OCT may also provide information about the pathology of the restenotic process by identifying features such as calcification or lipid content, which suggests neoatherosclerosis within the stent. In the following two cases, we highlight how the use of OCT can help to guide clinical decision-making when dealing with ISR.
other pathologies and can easily distinguish stent struts. OCT may also provide information about the pathology of the restenotic process by identifying features such as calcification or lipid content, which suggests neoatherosclerosis within the stent. In the following two cases, we highlight how the use of OCT can help to guide clinical decision-making when dealing with ISR.
Case 1
Age: 47
Gender: Male
History: Hypertension, hyperlipidaemia and previous smoking.
- Previous PCI to mid-LAD in 2009 and in 2010 at an outside hospital. The details of these previous PCIs were unknown and it was unclear how many stents had previously been placed.
- The patient presented to Mount Sinai with Canadian Cardiovascular Society (CCS) Class III angina. Exercise myocardial perfusion imaging revealed a small reversible apical perfusion defect.
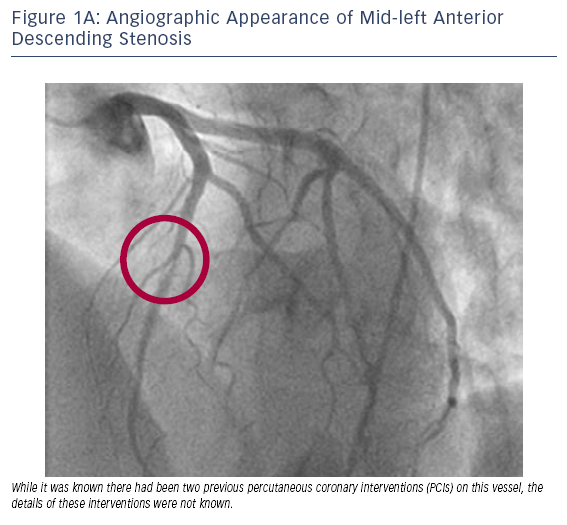
- Cardiac catheterisation suggested a stenosis in the mid-LAD region (see Figure 1A).
- As seen in Figure 1B, OCT of the stenotic LAD lesion identified two stent layers; both layers appeared to be well-apposed.
- Based on these OCT findings of well-apposed, double-layered stents, clinical decision-making was simplified, with reaso
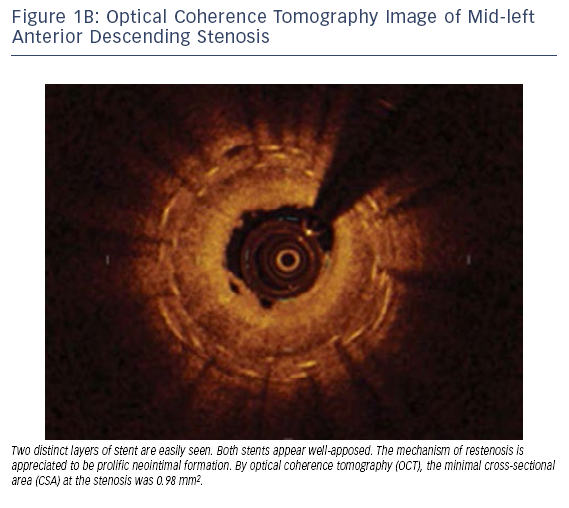 nable options including percutaneous transluminal coronary angioplasty (PTCA), bypass surgery or PTCA with potential brachytherapy.
nable options including percutaneous transluminal coronary angioplasty (PTCA), bypass surgery or PTCA with potential brachytherapy. - Following patient consultation with a cardiothoracic surgeon and interventional cardiologist, a cutting balloon PTCA was performed at 10 atmospheres followed by brachytherapy.
Notably, the high resolution of OCT was able to easily define the two layers of stent and prevented us from placing a third layer of stent in this patient.
Case 2
Age: 57
Gender: Male
History: Hypertension, diabetes and hyperlipidaemia.
- This patient was known to have had previous PCI to the distal RCA on two previous occasions with double-layered stents.
- The patient presented with recurrent CCS Class IV angin
 a while receiving four antianginal medications (nitrate, ranolazine, beta-blocker and calcium
a while receiving four antianginal medications (nitrate, ranolazine, beta-blocker and calcium 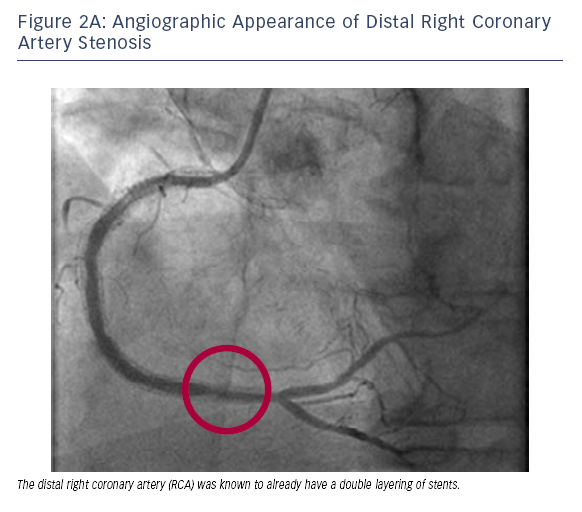 channel blocker).
channel blocker). - Cardiac catheterisation suggested a stenosis in the distal RCA (see Figure 2A).
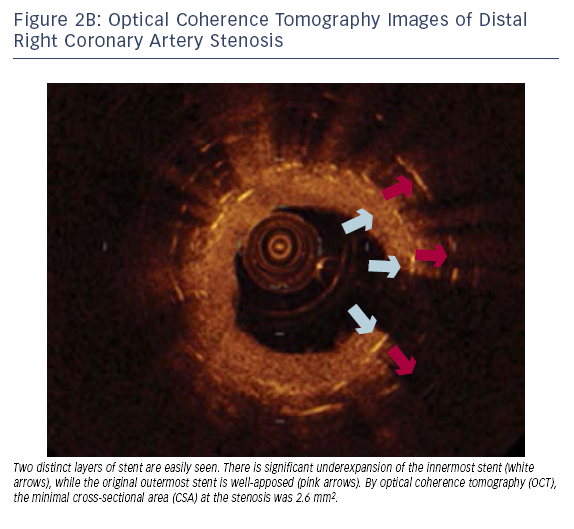
- OCT imaging of the distal RCA revealed that the innermost stent (most recently deployed) was significantly underexpanded (see Figure 2B).
- A high-pressure, non-compliant balloon was used to expand the inner stent.
- Unlike Case 1, and given the issue of suboptimal placement of the previous innermost stent with underexpansion, these options were considered preferable to bypass surgery or initial brachytherapy.
In this patient, the resolution of OCT was able to easily identify the two layers of stent and define underexpansion of the innermost stent as a significant issue.
 other pathologies and can easily distinguish stent struts. OCT may also provide information about the pathology of the restenotic process by identifying features such as calcification or lipid content, which suggests neoatherosclerosis within the stent. In the following two cases, we highlight how the use of OCT can help to guide clinical decision-making when dealing with ISR.
other pathologies and can easily distinguish stent struts. OCT may also provide information about the pathology of the restenotic process by identifying features such as calcification or lipid content, which suggests neoatherosclerosis within the stent. In the following two cases, we highlight how the use of OCT can help to guide clinical decision-making when dealing with ISR.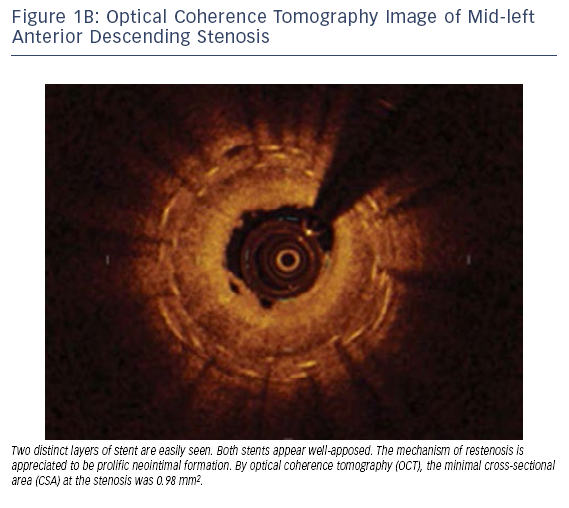 nable options including percutaneous transluminal coronary angioplasty (PTCA), bypass surgery or PTCA with potential brachytherapy.
nable options including percutaneous transluminal coronary angioplasty (PTCA), bypass surgery or PTCA with potential brachytherapy.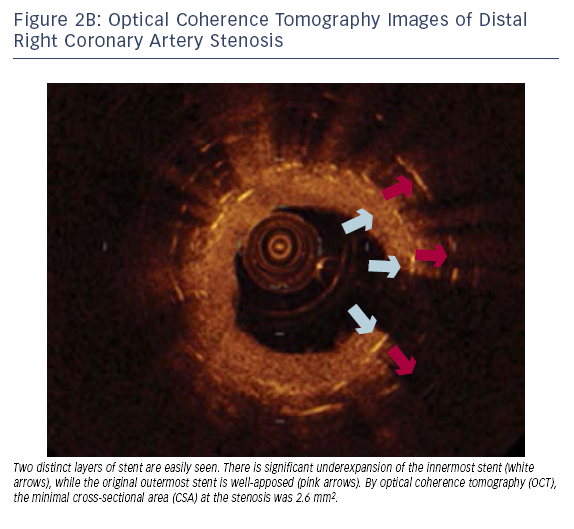 a while receiving four antianginal medications (nitrate, ranolazine, beta-blocker and calcium
a while receiving four antianginal medications (nitrate, ranolazine, beta-blocker and calcium 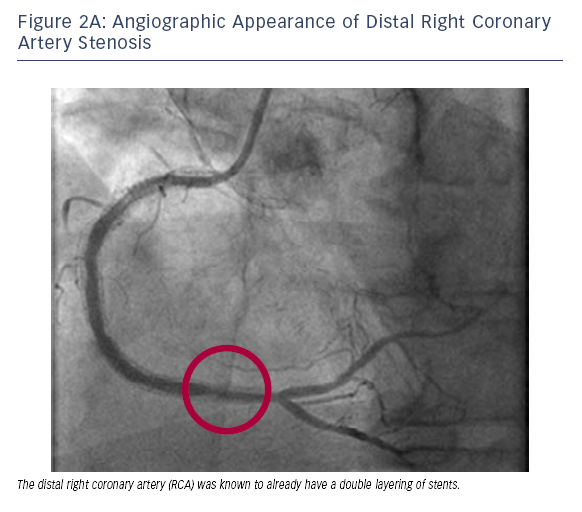 channel blocker).
channel blocker).