Scenario V – Stent Deployment and Edge Dissection 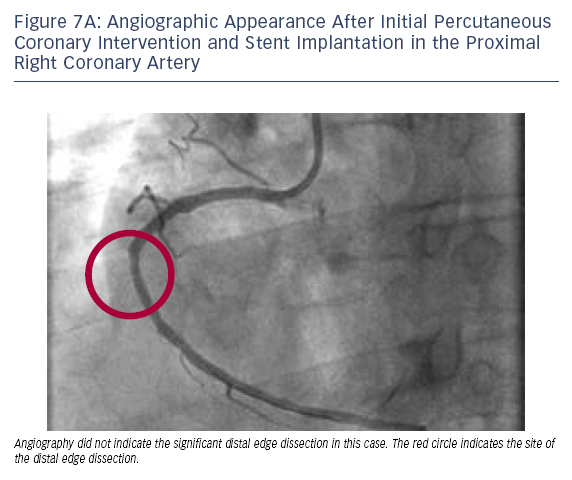
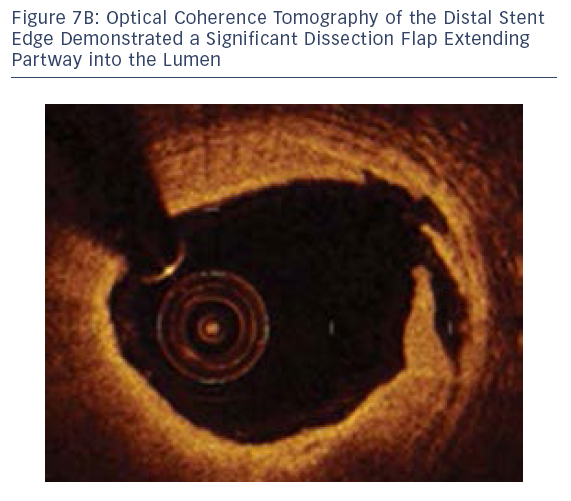
As an example of the utility of OCT and the superior resolution of this technology, it has become possible to diagnose potentially important problems after stent deployment; such as edge dissection, tissue prolapse or lack of lesion coverage. The significance of these findings remains to be demonstrated, although we have found it is not uncommon to find subtle examples of these problems after stent deployment that appear to be of little or no clinical consequence. However, when OCT imaging identifies a major problem after stent deployment, such as the case below, generally our practice is to address this issue.
Case 7
Age: 47
Gender: Male
History: Hypertension. Presented to an outside hospital and was ruled in for non-ST-segment myocardial infarction with a peak troponin I of 9.95 and an EKG showing inferior T-wave inversion.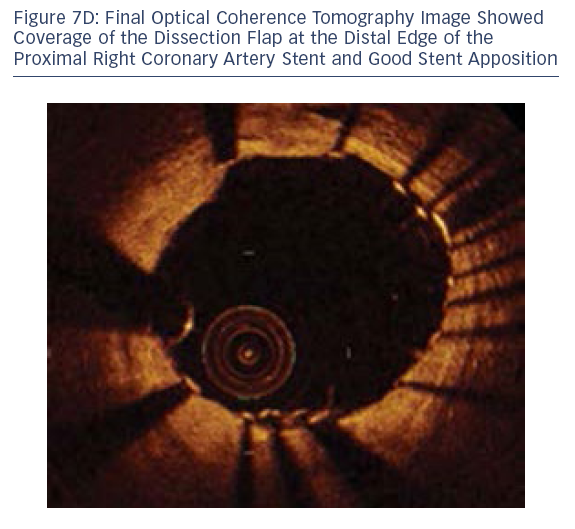
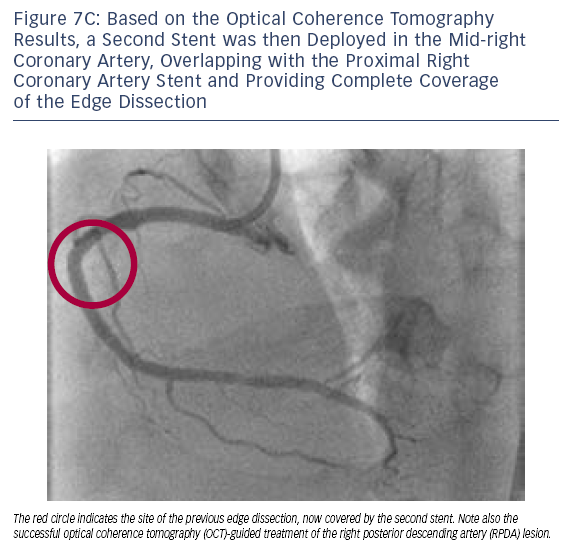
In this case, OCT was able to diagnose a significant distal edge dissection, guide the decision to implant a second stent and optimise PCI of the additional RPDA lesion.
The publication of this information was supported by St. Jude Medical.