Scenario VI – Bifurcation Lesion Assessment and Percutaneous 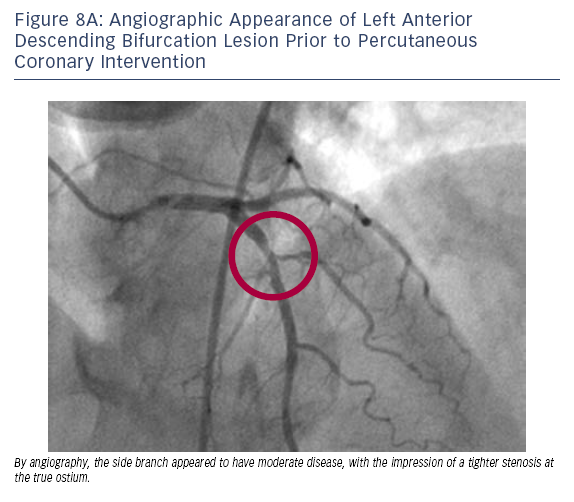
 Coronary Intervention
Coronary Intervention
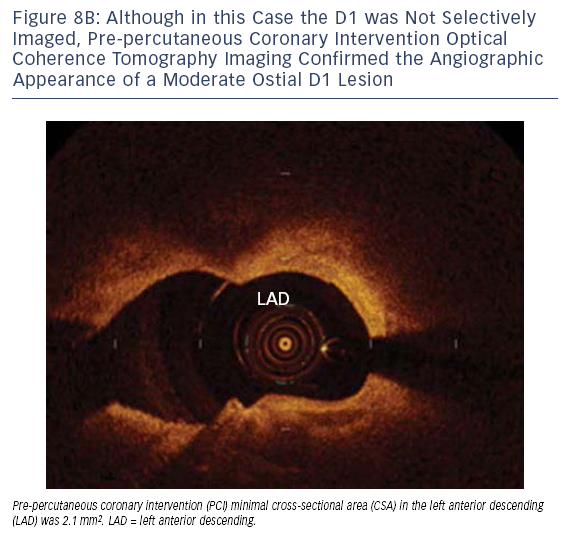
Bifurcation stenting remains one of the more technically challenging tasks in interventional cardiology. A major aspect in approaching a bifurcation PCI is choosing between a single versus a dual stent strategy. In our experience, lesion features most likely to require a two-stent approach include ostial side branch disease and a large diameter side branch (≥ 2.5 mm) subtending a large region of myocardium. OCT has the ability to assist in defining these characteristics and aid in the selection of a bifurcation stent strategy. It can also be of value for assessing the post-PCI result including any ‘pinch’ of the side branch ostium. While it often appears adequate to only perform OCT of the main vessel, prior to PCI we are increasingly performing OCT of both the main vessel and side branch, as we have found instances where main vessel imaging (by OCT, IVUS or other modality) does not adequately define the true side branch anatomy. If only a single vessel is to undergo pre-PCI OCT imaging, then imaging of the side branch is often the most informative and helpful in planning the PCI strategy.
Case 8
Age: 63
Gender: Female
History: Hypertension, hyperlipidaemia and asthma. Presented with progressive CCS Class III angina and was found to have a positive exercise EKG stress test.
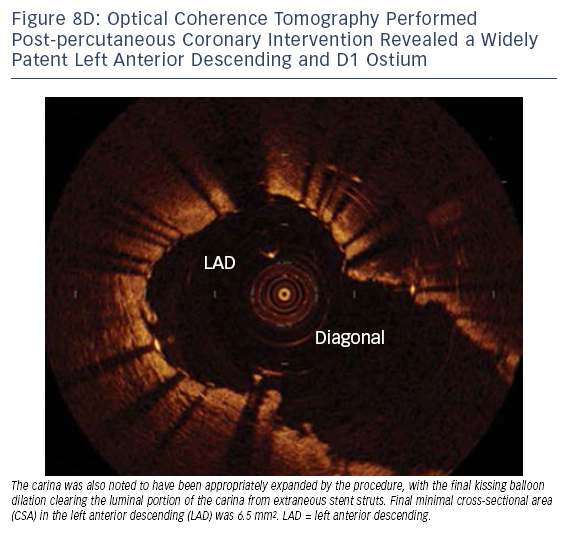
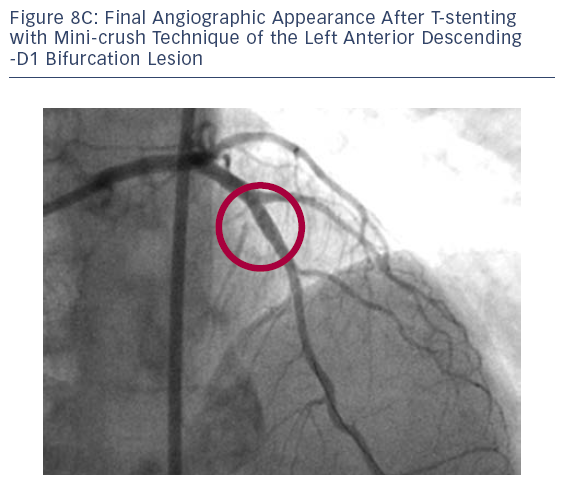
Although our preference is to perform OCT of both the side branch and main vessel, even by imaging only the main vessel OCT was able to aid in the correct selection of a bifurcation stent strategy and confirm proper expansion of the carina post-PCI.
The publication of this information was supported by St. Jude Medical.