Scenario III – Thrombosis
Plaque rupture with arterial thrombosis is the underlying event in most cases of acute coronary syndrome (ACS). Althou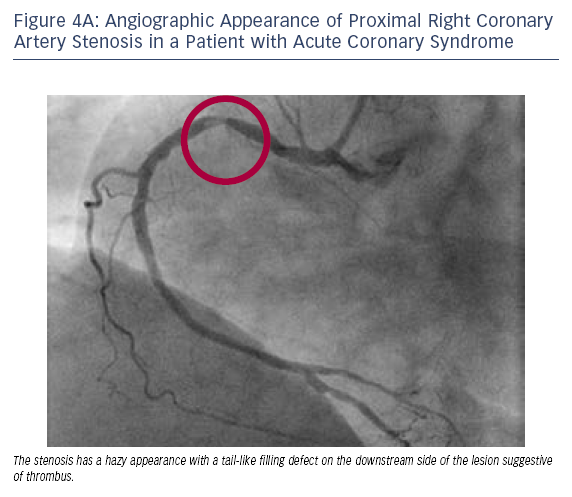 gh it is not necessary to perform OCT for the majority of PCIs performed in the setting of ACS, it is important to appreciate the excellent sensitivity of this imaging tool to detect intra-arterial thrombus. In certain cases, OCT can play an important role in guiding interventional decisionmaking with respect to thrombus burden and PCI. For example, in a patient with ACS and multiple lesions, OCT can be used to distinguish between a culprit lesion with fresh thrombus versus a chronic total occlusion. Prior to stent implantation, OCT can also assess the success of thrombus aspiration or disruption.
gh it is not necessary to perform OCT for the majority of PCIs performed in the setting of ACS, it is important to appreciate the excellent sensitivity of this imaging tool to detect intra-arterial thrombus. In certain cases, OCT can play an important role in guiding interventional decisionmaking with respect to thrombus burden and PCI. For example, in a patient with ACS and multiple lesions, OCT can be used to distinguish between a culprit lesion with fresh thrombus versus a chronic total occlusion. Prior to stent implantation, OCT can also assess the success of thrombus aspiration or disruption.
Case 4
Age: 51
Gender: Female
History: Hypertension and previous deep vein thrombosis. Presented with new onset, prolonged substernal chest pain at rest (CCS Class IV) and an elevated troponin I of 0.7, consistent with non-ST-segment myocardial infarction.
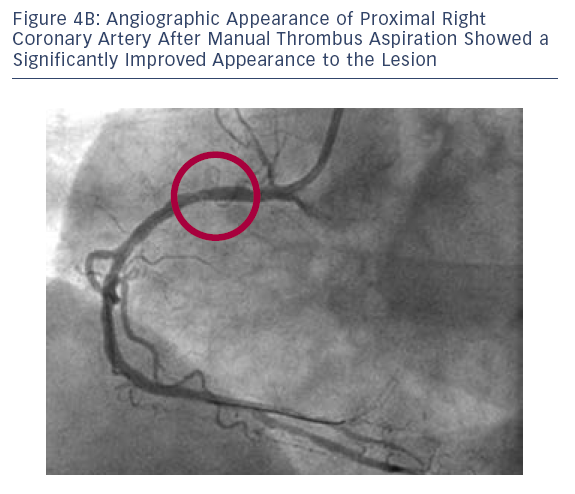 was used to reduce the thrombotic burden.
was used to reduce the thrombotic burden.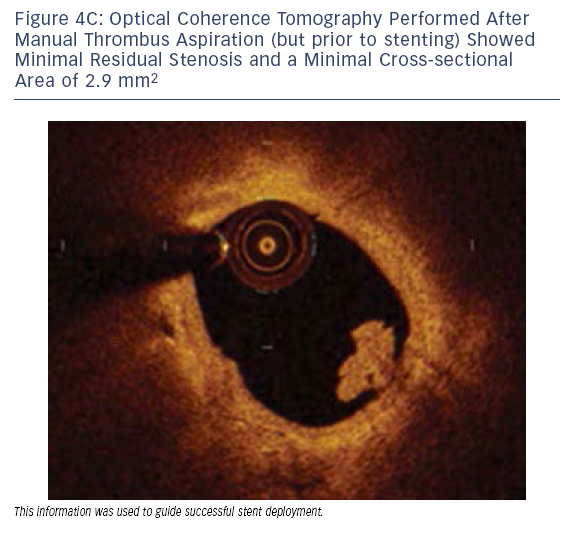
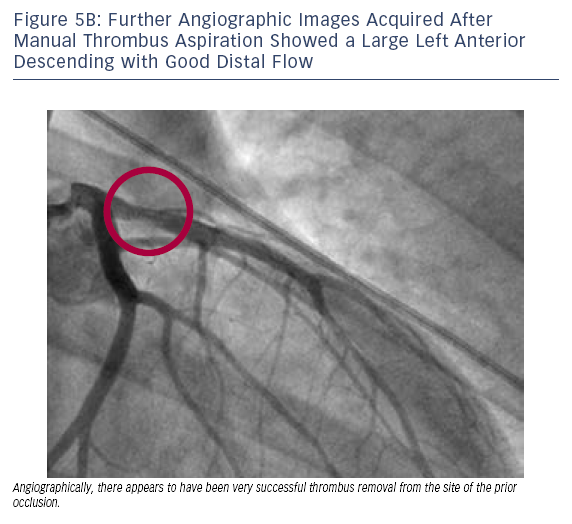
In this PCI case, OCT confirmed adequate thrombus removal prior to stenting, which helped to guide stent size by assessing lesion length and vessel diameter and, finally, confirming optimal stent deployment post-PCI.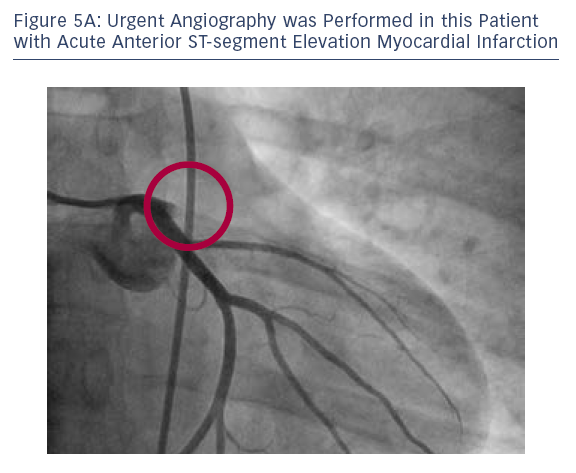
Case 5
Age: 33
Gender: Male
History: Coronary artery disease but no other cardiovascular risk factors. Presented with a four-hour history of severe chest pain and an electrocardiogram (EKG) consistent with an acute ST-segment elevation anterior myocardial infarction.
 d
d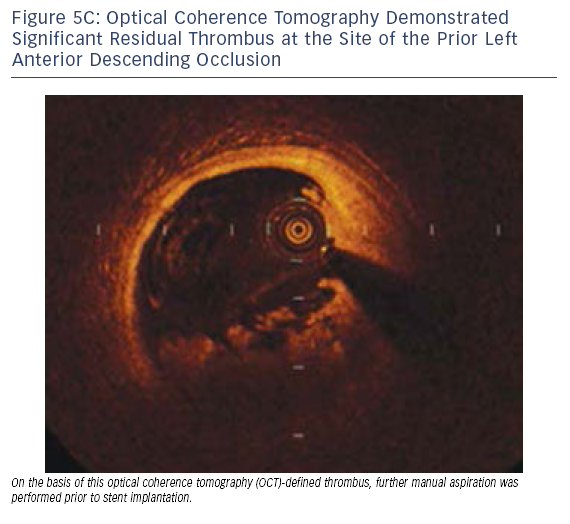 en (see Figure 5C).
en (see Figure 5C).Cases 4 and 5 highlight the use of OCT to define adequacy of thrombus removal prior to stent implantation. While the efficacy of this practice remains to be demonstrated in large clinical trials, the rationale is that distal embolisation is minimised by reducing the thrombus load at the time of stent deployment.
The publication of this information was supported by St. Jude Medical.