Summary
Scenario II – Assessment of Calcified Lesions
Calcification is another major problem faced in the cath lab. The ability to adequately assess and treat calcified lesions is cri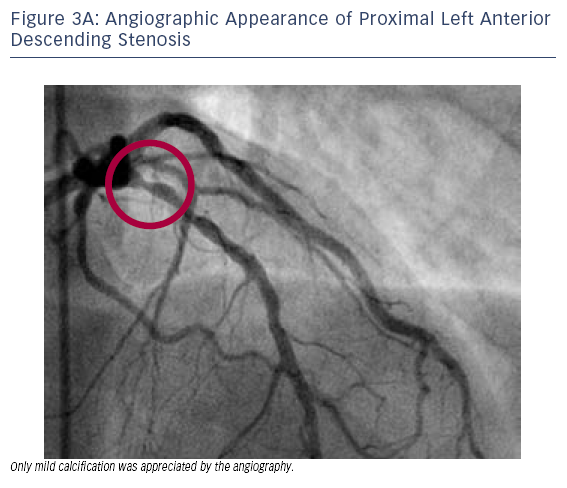 tical to the success of any PCI programme. While gross arterial calcification may be appreciated by fluoroscopy, in many instances calcification may be more subtle. Here, OCT can be invaluable for assessing these lesions and planning an appropriate PCI strategy.
tical to the success of any PCI programme. While gross arterial calcification may be appreciated by fluoroscopy, in many instances calcification may be more subtle. Here, OCT can be invaluable for assessing these lesions and planning an appropriate PCI strategy.
Case 3
Age: 47
Gender: Male
History: Hypertension, diabetes, hyperlipidaemia and smoking. Presented with CCS Class I angina and dyspnoea on exertion.
- Initial coronary computed tomography (CT) angiography performed by the patient’s primary care physician was suggestive of a stenosis of the LAD.
- Subsequent non-invasive nuclear stress testing was suggestive of inferior ischaemia; although balanced ischaemia involving other territories could not be excluded.
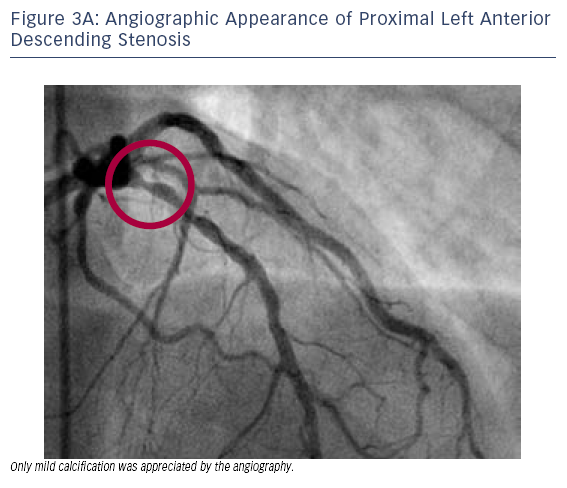
- Cardiac catheterisation revealed a segmental 70–80 % stenosis in the proximal LAD (Figure 3A) and total occlusion of the RCA. Only mild LAD calcification was appreciated based on the angiographic
 appearance.
appearance.
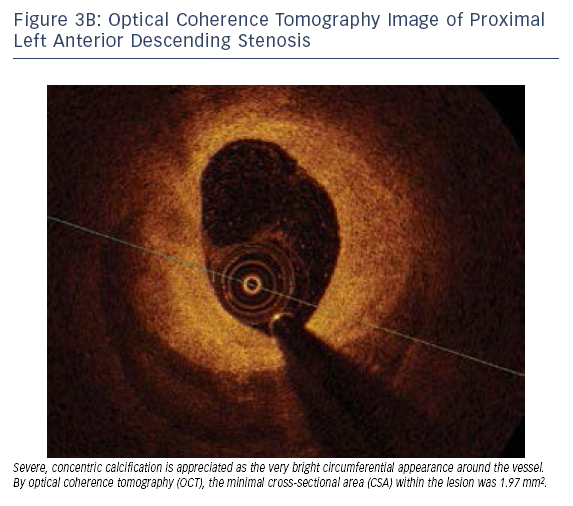
- As seen in Figure 3B, OCT of the stenotic LAD revealed severe concentric calcification with a minimal cross-sectional area (CSA) of 1.97 mm2.
- These findings were confirmed by intravascular ultrasound (IVUS) (see Figure 3C).
- Based on these OCT findings of severe concentric calcification, the lesion was treated by Rotablator™ rotational atherectomy system (Boston Scientific Corporation, Marlborough, MA, USA) prior to stent implantation.
In this case, OCT helped to define severe calcification and lesion severity, guiding the choice of an aggressive debulking strategy that was used to successfully treat this lesion.
 tical to the success of any PCI programme. While gross arterial calcification may be appreciated by fluoroscopy, in many instances calcification may be more subtle. Here, OCT can be invaluable for assessing these lesions and planning an appropriate PCI strategy.
tical to the success of any PCI programme. While gross arterial calcification may be appreciated by fluoroscopy, in many instances calcification may be more subtle. Here, OCT can be invaluable for assessing these lesions and planning an appropriate PCI strategy.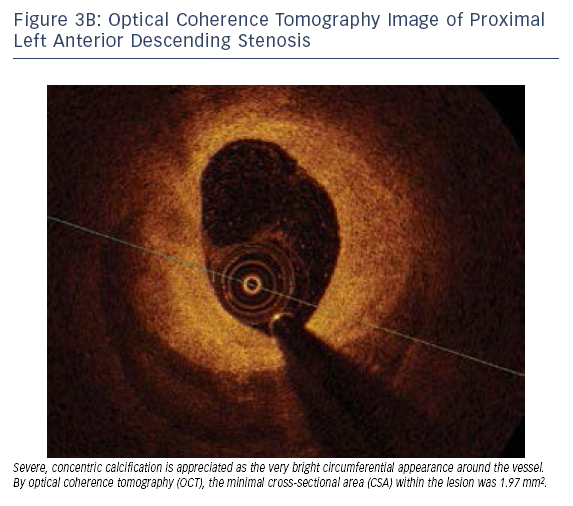 appearance.
appearance.